Michael Greger's Blog, page 12
September 10, 2024
Testing for Vitamin B12 Deficiency
Many doctors mistakenly rely on serum B12 levels in the blood to test for vitamin B12 deficiency.
There were two cases of young, strictly vegetarian individuals with no known vascular risk factors. One suffered a stroke, and the other had multiple strokes. Why? Most probably because they weren’t taking vitamin B12 supplements, which leads to high homocysteine levels, which can attack our arteries.
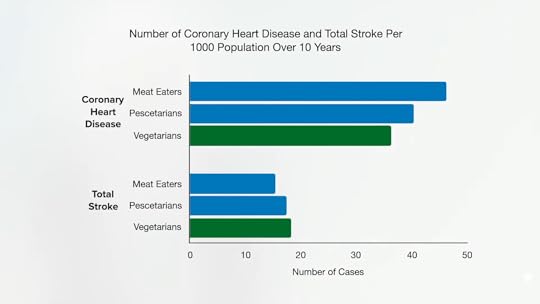
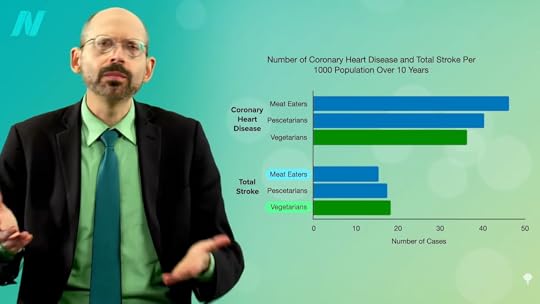
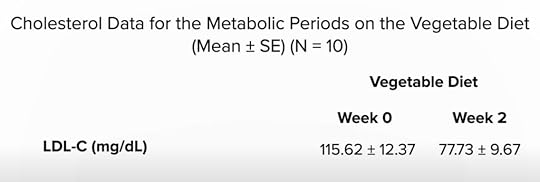
So, those eating plant-based who fail to supplement with B12 may increase their risk of both heart disease and stroke. However, as you can see in the graph below and at 0:47 in my video How to Test for Functional Vitamin B12 Deficiency, vegetarians have so many heart disease risk factor benefits that they are still at lower risk overall, but this may help explain why vegetarians were found to have more stroke. This disparity would presumably disappear with adequate B12 supplementation, and the benefit of lower heart disease risk would grow even larger.

Compared with non-vegetarians, vegetarians enjoy myriad other advantages, such as better cholesterol, blood pressure, blood sugars, and obesity rates. But, what about that stroke study? Even among studies that have shown benefits, “the effect was not as pronounced as expected, which may be a result of poor vitamin B12 status due to a vegetarian diet. Vitamin B12 deficiency may negate the cardiovascular disease prevention benefits of vegetarian diets. To further reduce the risk of cardiovascular disease, vegetarians should be advised to use vitamin B12 supplements.”
How can you determine your B12 status? By the time you’re symptomatic with B12 deficiency, it’s too late. And, initially, the symptoms can be so subtle that you might even miss them. What’s more, you develop metabolic vitamin B12 deficiency well before you develop a clinical deficiency, so there’s “a missed opportunity to prevent dementia and stroke” when you have enough B12 to avoid deficiency symptoms, but not enough to keep your homocysteine in check. “Underdiagnosis of this condition results largely from a failure to understand that a normal serum [blood level] B12 may not reflect an adequate functional B12 status.” The levels of B12 in our blood do not always represent the levels of B12 in our cells. We can have severe functional deficiency of B12 even though our blood levels are normal or even high.
“Most physicians tend to assume that if the serum B12 is ‘normal,’ there is no problem,” but, within the lower range of normal, 30 percent of patients could have metabolic B12 deficiency, with high homocysteine levels.
Directly measuring levels of methylmalonic acid (MMA) or homocysteine is a “more accurate reflection of vitamin B12 functional statuses.” Methylmalonic acid can be checked with a simple urine test; you’re looking for less than a value of 4 micrograms per milligram of creatinine. “Elevated MMA is a specific marker of vitamin B12 deficiency while Hcy [homocysteine] rises in both vitamin B12 and folate deficiencies.” So, “metabolic B12 deficiency is strictly defined by elevation of MMA levels or by elevation of Hcy in folate-replete individuals,” that is, in those getting enough folate. Even without eating beans and greens, which are packed with folate, folic acid is added to the flour supply by law, so, these days, high homocysteine levels may be mostly a B12 problem. Ideally, you’re looking for a homocysteine level in your blood down in the single digits.
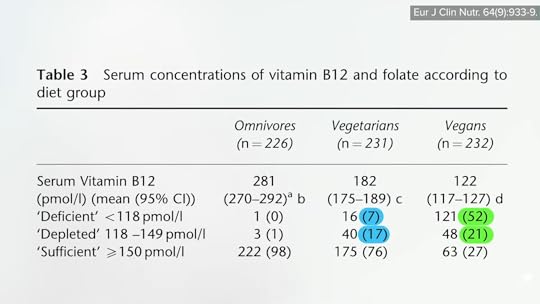
Measured this way, “the prevalence of subclinical functional vitamin B12 deficiency is dramatically higher than previously assumed…” We’re talking about 10 to 40 percent of the general population, more than 40 percent of vegetarians, and the majority of vegans who aren’t scrupulous about getting their B12. Some suggest that those on plant-based diets should check their vitamin B12 status every year, but you shouldn’t need to if you’re adequately supplementing.
There are rare cases of vitamin B12 deficiency that can’t be picked up on any test, so it’s better to just make sure you’re getting enough.
If you do get your homocysteine tested and it’s still too high, up in the double digits despite B12 supplementation and eating beans and greens, I have a suggestion for you in the final videos of this series, which we’ll turn to next with: Should Vegetarians Take Creatine to Normalize Homocysteine? and The Efficacy and Safety of Creatine for High Homocysteine.
How did we end up here? To watch the full series if you haven’t yet, check the related posts below.
September 5, 2024
What About Homocysteine, Vitamin B12, and Vegetarians’ Stroke Risk?
Not taking vitamin B12 supplements or regularly eating B12-fortified foods may explain the higher stroke risk found among vegetarians.
Leonardo da Vinci had a stroke. Might his vegetarian diet have been to blame? “His stroke…may have been related to an increase in homocysteine level because of the long duration of his vegetarian diet.” A suboptimal intake of vitamin B12 is common in those eating plant-based diets (unless they take B12 supplements or regularly eat B12-fortified foods) and can lead to an increased level of homocysteine in the blood, which “is accepted as an important risk factor for stroke.”
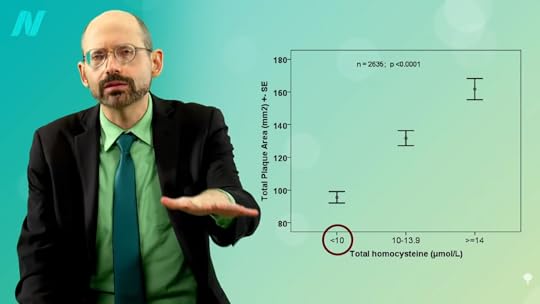
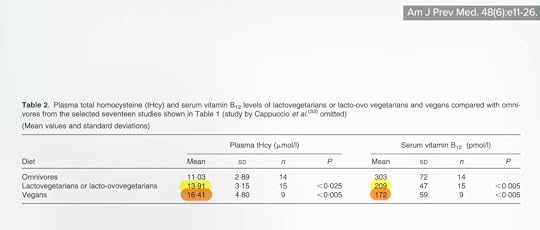
“Accepted” may be overstating it as there is still “a great controversy” surrounding the connection between homocysteine and stroke risk. But, as you can see in the graph below and at 0:57 in my video Vegetarians and Stroke Risk Factors: Vitamin B12 and Homocysteine?, those with higher homocysteine levels do seem to have more atherosclerosis in the carotid arteries that lead up to the brain, compared to those with single-digit homocysteine levels, and they also seem to be at higher risk for clotting ischemic strokes in observational studies and, more recently, bleeding hemorrhagic strokes, as well as increased risk of dying from cardiovascular disease and all causes put together.
Even more convincing are the genetic data. About 10 percent of the population has a gene that increases homocysteine levels by about 2 points, and they appear to have significantly higher odds of having a stroke. Most convincing would be randomized, double-blind, placebo-controlled trials to prove that lowering homocysteine with B vitamins can lower strokes, and, indeed, that appears to be the case for clotting strokes: Strokes with homocysteine-lowering interventions were more than five times as likely to reduce stroke compared with placebo.
Ironically, one of the arguments against the role of homocysteine in strokes is that, “assuming that vegetarians have lower vitamin B12 concentrations than meat-eaters and that low vitamin B12 concentrations cause ischaemic stroke, then the incidence of stroke should be increased among vegetarians…but this is not the case.” However, it has never been studied until now.
As you can see in the graph below and at 2:16 in my video, the EPIC-Oxford study researchers found that vegetarians do appear to be at higher risk.
And no wonder, as about a quarter of the vegetarians and nearly three-quarters of the vegans studied were vitamin B12-depleted or B12-deficient, as you can see below and at 2:23, and that resulted in extraordinarily high homocysteine levels.
Why was there so much B12 deficiency? Because only a small minority were taking a dedicated B12 supplement. And, unlike in the United States, B12 fortification of organic foods isn’t allowed in the United Kingdom. So, while U.S. soymilk and other products may be fortified with B12, UK products may not. We don’t see the same problem among U.S. vegans in the Adventist study, presumably because of the B12 fortification of commonly eaten foods in the United States. It may be no coincidence that the only study I was able to find that showed a significantly lower stroke mortality risk among vegetarians was an Adventist study.
Start eating strictly plant-based without B12-fortified foods or supplements, and B12 deficiency can develop. However, that was only for those not eating sufficient foods fortified with B12. Those eating plant-based who weren’t careful about getting a regular reliable source of B12 had lower B12 levels and, consequently, higher homocysteine levels, as you can see below and at 3:27 in my video.
The only way to prove vitamin B12 deficiency is a risk factor for cardiovascular disease in vegetarians is to put it to the test. When researchers measured the amount of atherosclerosis in the carotid arteries, the main arteries supplying the brain, “no significant difference” was found between vegetarians and nonvegetarians. They both looked just as bad even though vegetarians tend to have better risk factors, such as lower cholesterol and blood pressure. The researchers suggest that B12 deficiency plays a role, but how do they know? Some measures of artery function weren’t any better either. Again, they surmised that vitamin B12 deficiency was overwhelming the natural plant-based benefits. “The beneficial effects of vegetarian diets on lipids and blood glucose [cholesterol and blood sugars] need to be advocated, and efforts to correct vitamin B12 deficiency in vegetarian diets can never be overestimated.”
Sometimes vegetarians did even worse. Worse artery wall thickness and worse artery wall function, “raising concern, for the first time, about the vascular health of vegetarians”—more than a decade before the new stroke study. Yes, their B12 was low, and, yes, their homocysteine was high, “suggest[ing] that vitamin B12 deficiency in vegetarians might have adverse effects on their vascular health.” What we need, though, is an interventional study, where participants are given B12 to see if that fixes it, and here we go. The title of this double-blind, placebo-controlled, randomized crossover study gives it away: “Vitamin B-12 Supplementation Improves Arterial Function in Vegetarians with Subnormal Vitamin B-12 Status.” So, compromised vitamin B12 status among those eating more plant-based diets due to not taking B12 supplements or regularly eating vitamin B12-fortified foods may explain the higher stroke risk found among vegetarians.
Unfortunately, many vegetarians resist taking vitamin B12 supplements due to “misconceptions,” like “hold[ing] on to the old myth that deficiency of this vitamin is rare and occurs only in a small proportion of vegans.” “A common mistake is to think that the presence of dairy products and eggs in the diet, as in LOV [a lacto-ovo vegetarian diet], can still ensure a proper intake [of B12]…despite excluding animal flesh.”
Now that we may have nailed the cause, maybe “future studies with vegetarians should focus on identifying ways to convince vegetarians to take vitamin B12 supplements to prevent a deficiency routinely.”
I have updated my recommendation for B12 supplementation. I now suggest at least 2,000 mcg (µg) of cyanocobalamin once weekly, ideally as a chewable, sublingual, or liquid supplement taken on an empty stomach, or at least 50 mcg daily of supplemental cyanocobalamin. (You needn’t worry about taking too much.) You can also have servings of B12-fortified foods three times a day (at each meal), each containing at least 190% of the Daily Value listed on the nutrition facts label. (Based on the new labeling mandate that started on January 1, 2020, the target is 4.5 mcg three times a day.) Please note, though, that those older than the age of 65 have only one option: to take 1,000 micrograms a day.
We started this series on what to eat and not eat for stroke prevention, and whether vegetarians really have a higher stroke risk. Check related posts for the last few videos that looked at specific factors.
Stay tuned for:
How to Test for Functional Vitamin B12 Deficiency Should Vegetarians Take Creatine to Normalize Homocysteine? The Efficacy and Safety of Creatine for High HomocysteineSeptember 3, 2024
What About Animal Protein and Vegetarians’ Stroke Risk?
Might animal protein-induced increases in the cancer-promoting growth hormone IGF-1 help promote brain artery integrity?
In 2014, a study on stroke risk and dietary protein found that greater intake was associated with lower stroke risk and, further, that the animal protein appeared particularly protective. Might that help explain why, as shown in the graph below and at 0:31 in my video Vegetarians and Stroke Risk Factors: Animal Protein?, vegetarians were recently found to have a higher stroke rate than meat eaters?
Animal protein consumption increases the levels of a cancer-promoting growth hormone in the body known as IGF-1, insulin-like growth factor 1, which “accelerates the progression of precancerous changes to invasive lesions.” High blood concentrations are associated with increased risks of breast, colorectal, lung, and prostate cancers, potentially explaining the association between dairy milk intake and prostate cancer risk, for example. However, there are also IGF-1 receptors on blood vessels, so perhaps IGF-1 promotes cancer and brain artery integrity.
People who have strokes appear to have lower blood levels of IGF-1, but it could just be a consequence of the stroke rather than the cause. There weren’t any prospective studies over time until 2017 when researchers found that, indeed, higher IGF-1 levels were linked to a lower risk of stroke—but is it cause and effect? In mice, the answer seems to be yes, and in a petri dish, IGF-1 appears to boost the production of elastin, a stretchy protein that helps keep our arteries elastic. As you can see in the graph below and at 1:41 in my video, higher IGF-1 levels are associated with less artery stiffness, but people with acromegaly, like Andre the Giant, those with excessive levels of growth hormones like IGF-1, do not appear to have lower stroke rates, and a more recent study of dietary protein intake and risk of stroke that looked at a dozen studies of more than half a million people (compared to only seven studies with a quarter million in the previous analysis), found no association between dietary protein intake and the risk of stroke. If anything, dietary plant protein intake may decrease the risk of stroke.

However, those with high blood pressure who have low IGF-1 levels do appear to be at increased risk of developing atherosclerosis, which is the thickening of the artery walls leading up to the brain, but no such association was found in people with normal blood pressure. So, there may be “a cautionary lesson for vegans” here. Yes, a whole food, plant-based diet “can down-regulate IGF-1 activity” and may slow the human aging process, not to mention reduce the risk of some of the common cancers that plague the Western world. But, “perhaps the ‘take-home’ lesson should be that people who undertake to down-regulate IGF-1 activity [by cutting down on animal protein intake] as a pro-longevity measure should take particular care to control their blood pressure and preserve their cerebrovascular health [the health of the arteries in their brain] – in particular, they should keep salt intake relatively low while insuring an ample intake of potassium” to keep their blood pressures down. So, that means avoiding processed foods and avoiding added salt, and, in terms of potassium-rich foods, eating beans, sweet potatoes, and dark-green leafy vegetables.
Might this explain the higher stroke risk found among vegetarians? No—because dairy and egg whites are animal proteins, too. Only vegans have lower IGF-1 levels in both men and women, so low levels of IGF-1 can’t explain why higher rates of stroke were found in vegetarians. Then what is it? I think the best explanation for the mystery is something called homocysteine, which I cover next.
If you aren’t familiar with IGF-1, my videos Flashback Friday: Animal Protein Compared to Cigarette Smoking and How Not to Die from Cancer are good primers.
Beyond eating a plant-based diet, how else can we lower our blood pressure? Check out the chapter of hypertension in my book How Not to Die at your local public library.
This is the eighth video in a 12-part series on vegetarians’ stroke risk. If you missed any of the previous ones, check out the related posts below.
Coming up, we turn to what I think is actually going on:
Vegetarians and Stroke Risk Factors: Vitamin B12 and Homocysteine? How to Test for Functional Vitamin B12 Deficiency Should Vegetarians Take Creatine to Normalize Homocysteine? The Efficacy and Safety of Creatine for High HomocysteineAugust 29, 2024
What About Saturated Fat and Vegetarians’ Stroke Risk?
How can we explain the drop in stroke risk as the Japanese diet became westernized with more meat and dairy?
As Japan westernized, the country’s stroke rate plummeted, as you can see in the graph below and at 0:15 in my video Vegetarians and Stroke Risk Factors: Saturated Fat?.

Stroke had been a leading cause of death in Japan, but the mortality rate decreased sharply as they moved away from their traditional diets and started eating more like those in the West. Did the consumption of all that extra meat and dairy have a protective effect? After all, their intake of animal fat and animal protein was going up at the same time their stroke rates were going down, as shown below and at 0:35 in my video.

Commented a noted Loma Linda cardiology professor, “Protection from stroke by eating animal foods? Surely not!…Many vegetarians, like myself, have almost come to expect the data to indicate that they have an advantage, whatever the disease that is being considered. Thus, it is disquieting to find evidence in a quite different direction for at least one subtype of stroke.”
Can dietary saturated fat, like that found in meat and dairy, be beneficial in preventing stroke risk? There appeared to be a protective association—but only in East Asian populations, as you can see below and at 1:11 in my video.

High dietary saturated fat was found to be associated with a lower risk of stroke in Japanese but not in non-Japanese. So, what was it about the traditional Japanese diet that the westernization of their eating habits made things better when it came to stroke risk? Well, at the same time, their meat and dairy intake was going up, and their salt intake was going down, as you can see below and at 1:40.

The traditional Japanese diet was packed with salt. They had some of the highest salt intakes in the world, about a dozen spoonsful of salt a day. Before refrigeration became widely available, they ate all sorts of salted, pickled, and fermented foods from soy sauce to salted fish. In the areas with twice the salt intake, they had twice the stroke mortality, but when the salt intake dropped, so did the stroke death rates, because when the salt consumption went down, their blood pressure went down, too. High blood pressure is perhaps “the single most important potentially modifiable risk factor for stroke,” so it’s no big mystery why the westernization of the Japanese diet led to a drop in stroke risk.
When they abandoned their more traditional diets, their obesity rates went up and so did their diabetes and coronary artery disease, but, as they gave up the insanely high salt intake, their insanely high stroke rates correspondingly fell.
Stomach cancer is closely associated with excess salt intake. When you look at their stomach cancer rates, they came down beautifully as they westernized their diets away from salt-preserved foods, as you can see in the graph below and at 2:50 in my video.

But, of course, as they started eating more animal foods like dairy, their rates of fatal prostate cancer, for example, shot through the roof. Compared to Japan, the United States has 7 times more deaths from prostate cancer, 5 times more deadly breast cancer, 3 times more colon cancer and lymphoma mortality, and 6 to 12 times the death rate from heart disease, as you can see in the graph below and at 3:15 in my video. Yes, Japanese stroke and stomach cancer rates were higher, but they were also eating up to a quarter cup of salt a day.
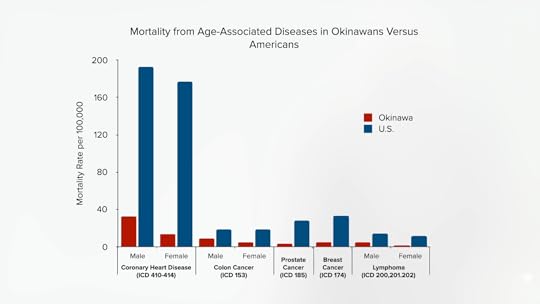
That would seem to be the most likely explanation, rather than some protective role of animal fat. And, indeed, it was eventually acknowledged in the official Japanese guidelines for the prevention of cardiovascular disease: “Refrain from the consumption of large amounts of fatty meat, animal fat, eggs, and processed foods…”
Now, one of the Harvard cohorts found a protective association between hemorrhagic strokes and both saturated fat and trans fat, prompting a “sigh of relief…heard throughout the cattle-producing Midwestern states,” even though the researchers concluded that, of course, we all have to cut down on animal fat and trans fat for the heart disease benefit. Looking at another major Harvard cohort, however, they found no such protective association for any kind of stroke, and when they put all the studies together, zero protection was found across the board, as you can see below and at 4:07 in my video.
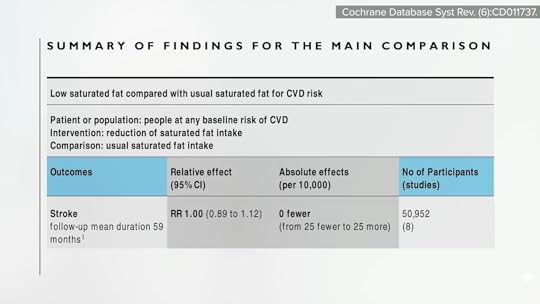
Observational studies have found that higher LDL cholesterol seems to be associated with a lower risk of hemorrhagic stroke, raising the possibility that cholesterol may be “a double-edged sword,” by decreasing the risk of ischemic stroke but increasing the risk of hemorrhagic stroke. But low cholesterol levels in the aged “may be a surrogate for nutritional deficiencies…or a sign of debilitating diseases,” or perhaps the individuals were on a combination of cholesterol-lowering drugs and blood thinners, and that’s why we tend to see more brain bleeds in those with low cholesterol. You don’t know until you put it to the test.
Researchers put together about two dozen randomized controlled trials and found that the lower your cholesterol, the better when it comes to overall stroke risk, with “no significant increase in hemorrhagic stroke risk with lower achieved low-density lipoprotein [LDL] cholesterol levels.”
The genetic data appear mixed, with some suggesting a lifetime of elevated LDL would give you a higher hemorrhagic stroke risk, while other data suggest more of that double-edged sword effect. However, with lower cholesterol, “any possible excess of hemorrhagic [bleeding] stroke is greatly outweighed by the protective effect against ischaemic stroke,” the much more common clotting type of stroke, not to mention heart disease. It may be on the order of 18 fewer clotting strokes for every 1 extra bleeding stroke with cholesterol-lowering.
Does this explain the increased stroke risk found among vegetarians? Hemorrhagic stroke is the type of stroke that appeared higher in vegetarians, but the cholesterol levels in vegans were even lower, and, if anything, vegans trended towards a higher clotting stroke risk, so it doesn’t make sense. If there is some protective factor in animal foods, it is to be hoped that a diet can be found that still protects against the killer number one, heart disease, without increasing the risk of the killer number five, stroke. But, first, we have to figure out what that factor is, and the hunt continues.
Aren’t there studies suggesting that saturated fat isn’t as bad as we used to think? Check out:
The Saturated Fat Studies: Set Up to Fail The Saturated Fat Studies: Buttering Up the Public Is Butter Really Back? What the Science SaysJust like the traditional Japanese diet had a lot going for it despite having high sodium as the fatal flaw, what might be the Achilles’ heel of plant-based diets when it comes to stroke risk?
This is the seventh video in this stroke series. See the related posts below for the others.
August 27, 2024
What About Vegan Junk Food and Vegetarians’ Stroke Risk?
Just because you’re eating a vegetarian or vegan diet doesn’t mean you’re eating healthfully.
“Plant-Based Diets Are Associated with a Lower Risk of Incident Cardiovascular Disease, Cardiovascular Disease Mortality, and All-Cause Mortality in a General Population of Middle-Aged Adults”: This study of a diverse sample of 12,000 Americans found that “progressively increasing the intake of plant foods by reducing the intake of animal foods is associated with benefits on cardiovascular health and mortality.” Still, regarding plant-based diets for cardiovascular disease prevention, “all plant foods are not created equal.” As you can see in the graph below and at 0:40 in my video Vegetarians and Stroke Risk Factors: Vegan Junk Food?, a British study found higher stroke risk in vegetarians. Were they just eating a lot of vegan junk food?

“Any diet devoid of animal food sources can be claimed to be a vegetarian [or vegan] diet; thus, it is important to determine” what is being eaten. One of the first things I look at when I’m trying to see how serious a population is about healthy eating is something that is undeniably, uncontroversially bad: soda, aka liquid candy. Anyone drinking straight sugar water doesn’t have health on top of mind.
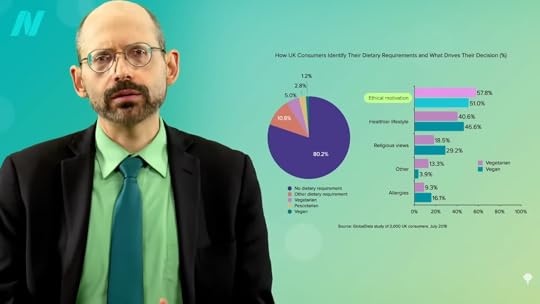
A large study was conducted of plant-based eaters in the United States, where people tend to cut down on meat for health reasons far more than for ethics, as you can see in the graph below and at 1:20 in my video.

Researchers found that flexitarians drink fewer sugary beverages than regular meat eaters, as do pescatarians, vegetarians, and vegans, as you can see below and at 1:30.
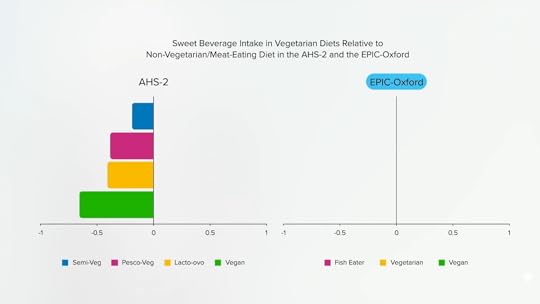
However, in the study from the United Kingdom where the increased stroke risk in vegetarians was found and where people are more likely to go veg or vegan for ethical reasons, researchers found that pescatarians drink less soda, but the vegetarians and vegans drink more, as shown in the graph below and at 1:44.

I’m not saying that’s why they had more strokes; it might just give us an idea of how healthfully they were eating. In the UK study, the vegetarian and vegan men and women ate about the same amounts of desserts, cookies, and chocolate, as you can see in the graph below and at 1:53.

They also consumed about the same total sugar, as shown below and at 2:02.

In the U.S. study, the average non-vegetarian is nearly obese, the vegetarians are a little overweight, and the vegans were the only ideal weight group. In this analysis of the UK study, however, everyone was about the same weight. The meat eaters were lighter than the vegans, as you can see below, and at 2:19 in my video. The EPIC-Oxford study seems to have attracted a particularly “health-conscious” group of meat eaters weighing substantially less than the general population.

Let’s look at some specific stroke-related nutrients. Dietary fiber appears to be beneficial for the prevention of cardiovascular disease, including stroke, and it seems the more, the better, as you can see in the graph below and at 2:43 in my video.
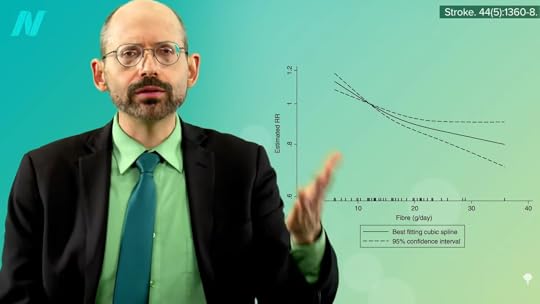
Based on studies of nearly half a million men and women, there doesn’t seem to be any upper threshold of benefit—so, again, “the more, the better.” At more than 25 grams of soluble fiber and 47 grams of insoluble dietary fiber, you can start seeing a significant drop in associated stroke risk. So, one could consider these values “as the minimal recommendable daily intake of soluble and insoluble fiber…to prevent stroke at a population level.” That’s what you see in people eating diets centered around minimally processed plant foods. Dean Ornish, M.D., got up around there with his whole food, plant-based diet. It might not be as much as we were designed to eat, based on the analyses of fossilized feces, but that’s about where we might expect significantly lower stroke risk, as shown below and at 3:25 in my video.

How much were the UK vegetarians getting? 22.1 grams. Now, in the UK, they measure fiber a little differently, so it may be closer to 30 grams, but that’s still not the optimal level for stroke prevention. It’s so little fiber that the vegetarians and vegans only beat out the meat eaters by about one or two bowel movements a week, as you can see below and at 3:48 in my video, suggesting the non-meat eaters were eating lots of processed foods.

The vegetarians were only eating about half a serving more of fruits and vegetables. Intake is thought to reduce stroke risk in part because of their potassium content, but the UK vegetarians at higher stroke risk were eating so few greens and beans that they couldn’t even match the meat eaters. The vegetarians (and the meat eaters) weren’t even reaching the recommended minimum daily potassium intake of 4,700 mg a day.
What about sodium? “The vast majority of the available evidence indicates that elevated salt intake is associated with higher stroke risk…” There is practically a straight-line increase in the risk of dying from a stroke, the more salt you eat, as you can see in the graph below and at 4:29 in my video.

Even just lowering sodium intake by a tiny fraction every year could prevent tens of thousands of fatal strokes. “Reducing Sodium Intake to Prevent Stroke: Time for Action, Not Hesitation” was the title of the paper, but the UK vegetarians and vegans appeared to be hesitating, as did the other dietary groups. “All groups exceeded the advised less than 2400 mg daily sodium intake”—and that didn’t even account for salt added to the table! The American Heart Association recommends less than 1,500 mg a day. So, they were all eating a lot of processed foods. It’s no wonder the vegetarians’ blood pressures were only one or two points lower. High blood pressure is perhaps “the single most important potentially modifiable risk factor for stroke.”
What evidence do I have that the vegetarians’ and vegans’ stroke risk would go down if they ate more healthfully? Well, in rural Africa, where they were able to nail the fiber intake that our bodies were designed to get by eating so many whole, healthy plant foods—including fruits, vegetables, grains, greens, beans, and protein almost entirely from plant sources—not only was heart disease, our number one killer, “almost non-existent,” but so was stroke. It only surged up from nowhere “with the introduction of salt and refined foods” to their diet.
“It is notable that stroke and senile dementia appear to be virtually absent in Kitava, an Oceanic culture [near Australia] whose quasi-vegan traditional diet is very low in salt and very rich in potassium.” They ate fish a few times a week, but the other 95 percent or so of their diet was made up of vegetables, fruits, corn, and beans. They had an apparent absence of stroke, even despite their ridiculously high rates of smoking, 76 percent of men and 80 percent of women. We evolved by eating as little as less than an eighth of a teaspoon of salt a day, and our daily potassium consumption is thought to have been as high as 10,000 mg or so. We went from an unsalted, whole-food diet to eating salty, processed foods depleted of potassium whether we eat meat or not.
Caldwell Esselstyn at the Cleveland Clinic tried putting about 200 patients with established cardiovascular disease on a whole food, plant-based diet. Of the 177 who stuck with the diet, only a single patient went on to have a stroke in the subsequent few years, compared to a hundred-fold greater rate of adverse events, including multiple strokes and deaths in those who strayed from the diet. “This is not vegetarianism,” Esselstyn explains. Vegetarians can eat a lot of less-than-ideal foods, “such as milk, cream, butter, cheese, ice cream, and eggs. This new paradigm is exclusively plant-based nutrition.”
This entire train of thought—that the reason typical vegetarians don’t have better stroke statistics is because they’re not eating particularly stellar diets—may explain why they don’t have significantly lower stroke rates. However, it still doesn’t explain why they may have higher stroke rates. Even if they’re eating similarly crappy, salty, processed diets, at least they aren’t eating meat, which we know increases stroke risk. There must be something about vegetarian diets that so increases stroke risk that it offsets their inherent advantages. We’ll continue our hunt for the answer next.
From a medical standpoint, labels like vegan and vegetarian just tell me what you don’t eat. It’s like identifying yourself as a “No-Twinkie-tarian.” You don’t eat Twinkies? Great, but what’s the rest of your diet like?
What are the healthiest foods? Check out my Daily Dozen.
To catch up on the rest of this series, see related posts below.
August 22, 2024
What About Omega-3s and Vegetarians’ Stroke Risk?
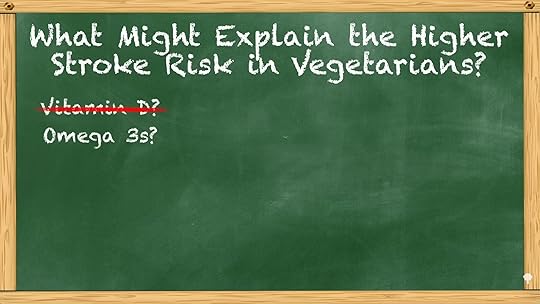
Does eating fish or taking fish oil supplements reduce stroke risk?
In my last video, we started to explore what might explain the higher stroke risk in vegetarians found in the EPIC-Oxford study. As you can see below and at 0:25 in my video Vegetarians and Stroke Risk Factors: Omega-3s?, vegetarians have a lower risk of heart disease and cardiovascular disease overall, but a higher risk of stroke. We looked into vitamin D levels as a potential mechanism, but that didn’t seem to be the reason. What about long-chain omega-3s, the fish fats like EPA and DHA?
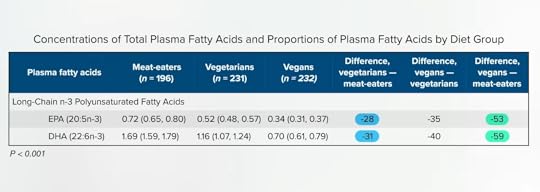
Not surprisingly, their levels are found to be “markedly lower in vegetarians and particularly in vegans than in meat-eaters.” They’re about 30 percent lower in vegetarians and more than half as low in vegans, as you can see below and at 0:45 in my video.
According to “the most extensive systematic assessment of effects of omega-3 fats on cardiovascular health to date,” combining 28 randomized controlled trials, stroke has no benefit. There is evidence that taking fish oil “does not reduce heart disease, stroke or death,” or overall mortality, either. This may be because, on the one hand, the omega-3s may be helping, but the mercury in fish may be making things worse. “Balancing the benefits with the contaminant risks of fish consumption has represented a challenge for regulatory agencies and public health professionals.”
For example, dietary exposure to polychlorinated biphenyls (PCBs) may be associated with an increased risk of stroke. In one study, for instance, “neither fish nor intake of PCBs was related to stroke risk. However, with adjustment for fish intake,” that is, at the same fish intake, “dietary PCBs were associated with an increased risk of total stroke,” so the PCB pollutants may be masking the fish benefit. If we had a time machine and could go back before the Industrial Revolution and find fish in an unpolluted state, we might find that it is protective against stroke. Still, looking at the EPIC-Oxford study data, if fish were protective, then we might expect that the pescatarians (those who eat fish but no other meat) would have lower numbers of strokes since they would have the fish benefit without the risk from other meat. But, no. That isn’t the reality. So, it doesn’t seem to be the omega-3s either.
Let’s take a closer look at what the vegetarians are eating.
When it comes to plant-based diets for cardiovascular disease prevention, all plant foods are not created equal. There are two types of vegetarians—those who do it for their health, and those who do it for ethical reasons, like global warming or animals—and the latter tend to eat different diets. Health vegans tend to eat more fruits and fewer sweets, for instance, and you don’t tend to see them chomping down on vegan donuts, as shown below and at 2:41 in my video.

“Concerns about health and costs were primary motivations for [meat] reduction” in the United States. A middle-class American family is four times more likely to reduce meat for health reasons compared to environmental or animal welfare concerns, as you can see in the graph below and at 2:55 in my video.

But in the United Kingdom, where the EPIC-Oxford stroke study was done, ethics was the number one reason given for becoming vegetarian or vegan, as you can see in below and at 3:05 in my video.
We know that “plant-based diets, diets that emphasize higher intakes of plant foods and lower intakes of animal foods, are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality”—a lower risk of dying from all causes put together—“in a general US adult population.” But, that’s only for healthy plant foods. Eating a lot of Wonder Bread, soda, and apple pie isn’t going to do you any favors. “For all types of plant-based diets, however, it is crucial that the choice of plant foods is given careful consideration.” We should choose whole fruits and whole grains over refined grains and avoid trans fats and added sugars. Could it be that the veggie Brits were just eating more chips? We’ll find out next.
Another strikeout trying to explain the increased risk. Could it be that the vegetarians were eating particularly unhealthy diets? Labels like vegetarian or vegan just tell me what is not being eaten. You can be vegetarian and consume a lot of unhealthy fare, like french fries, potato chips, and soda. That’s why, as a physician, I prefer the term whole food, plant-based nutrition. That tells me what you do eat. You eat vegetables and follow a diet centered around the healthiest foods out there.
If you missed the first four videos in this series, see:
What to Eat for Stroke Prevention What Not to Eat for Stroke Prevention Do Vegetarians Really Have Higher Stroke Risk? Vegetarians and Stroke Risk Factors: Vitamin D?Surprised about the fishy oil findings? Learn more: Is Fish Oil Just Snake Oil? and Omega-3s and the Eskimo Fish Tale.
August 20, 2024
What About Vitamin D and Vegetarians’ Stroke Risk?
Could the apparent increased stroke risk in vegetarians be reverse causation? And what about vegetarians versus vegans?
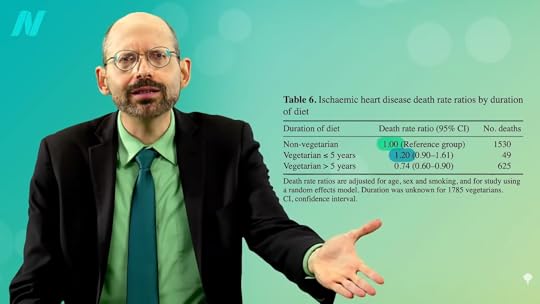
In the “Risks of Ischaemic Heart Disease and Stroke in Meat Eaters, Fish Eaters, and Vegetarians Over 18 Years of Follow-Up” EPIC-Oxford study, not surprisingly, vegetarian diets were associated with less heart disease—10 fewer cases per 1,000 people per decade compared to meat eaters—but vegetarian diets were associated with three more cases of stroke. So, eating vegetarian appears to lower the risk of cardiovascular disease by 7 overall, but why the extra stroke risk? Could it just be reverse causation?
When studies have shown higher mortality among those who quit smoking compared to people who continue to smoke, for example, we suspect “reverse causality.” When we see a link between quitting smoking and dying, instead of quitting smoking leading to people dying, it’s more likely that being “affected by some life-threatening condition” led people to quit smoking. It’s the same reason why non-drinkers can appear to have more liver cirrhosis; their failing liver led them to stop drinking. This is the “sick-quitter effect,” and you can see it when people quit meat, too.
As you can see below and at 1:16 in my video Vegetarians and Stroke Risk Factors: Vitamin D?
, new vegetarians can appear to have more heart disease than non-vegetarians. Why might an older person all of a sudden start eating vegetarian? Well, they may have just been diagnosed with heart disease, so that may be why there appear to be higher rates for new vegetarians—an example of the sick-quitter effect. To control for that, you can throw out the first five years of data to make sure the diet has a chance to start working. And, indeed, when you do that, the true effect is clear: a significant drop in heart disease risk.
So, does that explain the apparent increased stroke risk, too? No, because researchers still found higher stroke risk even after the first five years of data were skipped. What’s going on? Let’s dive deeper into the data to look for clues.
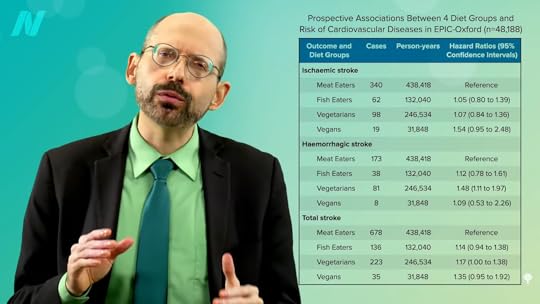
What happens when you break down the results by type of stroke and type of vegetarian (vegetarian versus vegan)? As you can see below and at 2:09 in my video, there are two main types of strokes—ischemic and hemorrhagic. Most common are ischemic, clotting strokes where an artery in the brain gets clogged off, as opposed to hemorrhagic, or bleeding strokes, where a blood vessel in the brain ruptures. In the United States, for example, it is about 90:10, with nine out of ten strokes the clotting (ischemic) type and one out of ten bleeding (hemorrhagic), the latter being the kind of stroke vegetarians appeared to have significantly more of. Now, statistically, the vegans didn’t have a significantly higher risk of any kind of stroke, but that’s terrible news for vegans. Do vegans have the same stroke risk as meat eaters? What is elevating their stroke risk so much that it’s offsetting all their natural advantages? The same could be said for vegetarians, too.
Even though this was the first study of vegetarian stroke incidence, there have been about half a dozen studies on stroke mortality. The various meta-analyses have consistently found significantly lower heart disease risk for vegetarians, but the lower stroke mortality was not statistically significant. Now, there is a new study that can give vegetarians some comfort in the fact that they at least don’t have a higher risk of dying from stroke, but that’s terrible news for vegetarians. Statistically, vegetarians have the same stroke death rate as meat eaters. Again, what’s going on? What is elevating their stroke risk so much that it’s offsetting all their natural advantages?
Let’s run through a couple of possibilities. As you can see in the graph below and at 3:48 in my video, if you look at the vitamin D levels of vegetarians and vegans, they tend to run consistently lower than meat eaters, and lower vitamin D status is associated with an increased risk of stroke. But who has higher levels of the sunshine vitamin? Those who are running around outside and exercising, so maybe that’s why their stroke risk is better. What we need are randomized studies.
When you look at people who have been effectively randomized at birth to genetically have lifelong, lower vitamin D levels, you do not see a clear indicator of increased stroke risk, so the link between vitamin D and stroke is probably not cause-and-effect.

We’ll explore some other possibilities, next.
So far in this series, we’ve looked at what to eat and what not to eat for stroke prevention, and whether vegetarians do have a higher stroke risk.
It may be worth reiterating that vegetarians do not have a higher risk of dying from a stroke, but they do appear to be at higher risk of having a stroke. How is that possible? Meat is a risk factor for stroke, so how could cutting out meat lead to more strokes? There must be something about eating plant-based that so increases stroke risk that it counterbalances the meat-free benefit. Might it be because plant-based eaters don’t eat fish? We turn to omega-3s next. For other videos in this series, see related posts below.
There certainly are benefits to vitamin D, though. Here is a sampling of videos where I explore the evidence.
August 15, 2024
The 411 on Statins
The cholesterol-lowering statin drug Lipitor has become the best-selling drug of all time, generating more than $140 billion in global sales. This class of drugs garnered so much enthusiasm in the medical community that some U.S. health authorities facetiously proposed they be added to the public water supply like fluoride is. One cardiology journal even offered the tongue-in-cheek suggestion for fast-food restaurants to offer “MacStatin” [sic] condiments along with ketchup packets to help neutralize the effects of unhealthy dietary choices.
What Are Statins and How Do They Work?Statins are drugs that can lower cholesterol. They work by blocking a substance that our body requires to make cholesterol.
Are Statins Bad for You?Although statins may be effective at lowering cholesterol and potentially helping to reduce the risk of heart disease and even stroke, they come with a host of possible side effects that may do much more harm than good.
What Possible Side Effects?As I discuss in the video Who Should Take Statins?, muscle-related side effects from cholesterol-lowering statin drugs “are often severe enough [to make] patients stop taking [them]. Of course, these side effects could be coincidental or psychosomatic and nothing to do with the drug,” given that many clinical trials show such side effects are rare. Of course, it is also possible that studies funded by the drug companies themselves may under-report side effects. The bottom line is that there’s an urgent need to establish the true incidence of statin side effects.
Researchers have found that those taking statins are significantly more likely to develop type 2 diabetes than those randomized to placebo sugar pills. Why? We’re still not exactly sure, but statins may have the double-whammy effect of impairing insulin secretion from the pancreas, as well as diminishing insulin’s effectiveness by increasing insulin resistance.
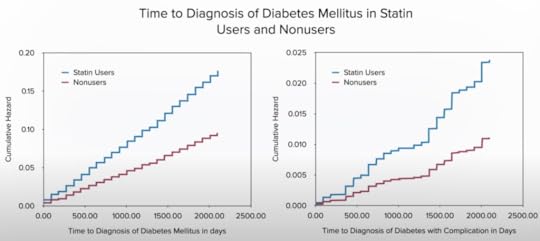
Even short-term statin use may approximately “double the odds of developing diabetes and diabetic complications,” and increased risks may persist for years after stopping statins.
Who Should Take Statins?How should you decide if a statin is right for you? “If you have a history of heart disease or stroke, taking a statin medication is recommended.” Period. Full stop. No discussion needed. However, if you don’t have any known cardiovascular disease, then the decision should be based on calculating your own personal risk, which you can easily do online if you know your cholesterol and blood pressure numbers, with the American College of Cardiology risk estimator or the Framingham risk profiler. (My favorite is the ACC estimator because it gives your current ten-year risk, as well as your lifetime risk.)
Under the current guidelines, if your ten-year risk is below 5 percent, unless there are extenuating circumstances, you should stick to diet, exercise, and smoking cessation to bring down your numbers. In contrast, if your ten-year risk hits or exceeds 20 percent, then the recommendation is to add a statin drug on top of making lifestyle modifications. Under 7.5 percent, the tendency is to stick with lifestyle changes unless there are risk-enhancing factors; above 7.5 percent, move towards adding drugs. What are the risk-enhancing factors to take into account when making the decision? A bad family history, really high LDL, metabolic syndrome, chronic kidney or inflammatory conditions, and persistently high triglycerides, C-reactive protein, or LP(a).
Relative Risk vs. Absolute RiskOne of the problems with communicating statin evidence to support shared decision-making is that most doctors have a poor understanding of concepts of risk, probability, and statistics, but that understanding is critical for preventive medicine. As discussed in my video Are Doctors Misleading Patients About Statin Risks and Benefits?, when doctors offer a cholesterol-lowering drug, they’re doing something quite different from treating a patient who is sick.
When drug companies say a statin reduces the risk of a heart attack by 36 percent, that’s the relative risk. In a large clinical study, 3 percent of patients not taking the statin drug had a heart attack within a certain amount of time, compared to 2 percent taking the drug. So, the drug dropped heart attack risk from about 3 percent to 2 percent, which is about a one-third drop—hence, the 36 percent reduced relative risk statistic. Another way to look at the change from 3 percent to 2 percent is that the absolute risk only dropped 1 percent. So, in effect, one’s chance of avoiding a heart attack over the next few years may be about 97 percent without treatment, but it can be increased to about 98 percent by taking daily statin drug. Yet another way to look at it: A hundred people would need to take the drug to prevent a single heart attack.
The Myth vs. the RealityIf you ask patients what they were led to believe, they think the chance of avoiding a heart attack within a few years on statins is 1 in 2, when it’s really 1 in a 100. And, if you ask, they want an absolute risk reduction of at least 30 percent or so to take a cholesterol-lowering drug every day, whereas the actual absolute risk reduction is only about 1 percent. So, the dirty little secret is that if patients knew the truth about how little these drugs actually worked, almost no one would agree to take them. So, doctors are either not educating their patients or they’re actively misinforming them.
Weighing the Risks and Benefits of StatinsIf all those numbers are blurring together, the Mayo Clinic developed a great visualization tool. For individuals at average risk who do not take a daily statin, 10 out of 100 may have a heart attack over the next ten years. However, if all 100 people took a statin every day for those ten years, 8 would have a heart attack and 2 would be spared. That’s about a 1 in 50 chance that taking the drug would help you avert a heart attack over the next decade. What if you have no known heart disease and you take statins for a few years? The chance statins will actually save your life is about 1 in 250.
What are the downsides? The cost and inconvenience of taking a pill every day, which can cause some gastrointestinal side effects, muscle aching and stiffness in maybe 5 percent, reversible liver inflammation in 2 percent, and more serious damage in perhaps 1 in 20,000 patients.

If you want a more personalized approach, calculate your ten-year risk. I cover this in more detail in my video The True Benefits vs. Side Effects of Statins.
Alternatives to Statins?As I discuss in my video How Much Longer Do You Live on Statins?, taking statins can enable you to live years longer because, for every millimole per liter you drop your bad LDL cholesterol, you may live three or even six years longer, depending on which study you’re reading. A millimole in U.S. units (mg/dL) is 39 points. Drop your LDL cholesterol about 39 mg/dL or 1 mmol/L, and you could live years longer. Exercise your whole life, and you may only increase your lifespan by six months, whereas stopping smoking may net you nine months. So, how can you drop your LDL cholesterol by about 39 points? You can accomplish that by taking drugs every day, or you can achieve that within just two weeks of eating a diet packed with fruits, vegetables, and nuts.
A plant-based diet has been shown to substantially reduce cholesterol levels and cardiovascular risk, as well as obesity, hypertension, and systemic inflammation—without negative side effects.
August 13, 2024
The Stroke Risk of Vegetarians
The first study in history on the incidence of stroke in vegetarians and vegans suggests they may be at higher risk.
“When ranked in order of importance, among the interventions available to prevent stroke, the three most important are probably diet, smoking cessation, and blood pressure control.” Most of us these days are doing pretty good about not smoking, but less than half of us exercise enough. And, according to the American Heart Association, only 1 in 1,000 Americans is eating a healthy diet and less than 1 in 10 is even eating a moderately healthy diet, as you can see in the graph below and at 0:41 in my video Do Vegetarians Really Have Higher Stroke Risk?. Why does it matter? It matters because “diet is an important part of stroke prevention. Reducing sodium intake, avoiding egg yolks, limiting the intake of animal flesh (particularly red meat), and increasing the intake of whole grains, fruits, vegetables, and lentils….Like the sugar industry, the meat and egg industries spend hundreds of millions of dollars on propaganda, unfortunately with great success.”
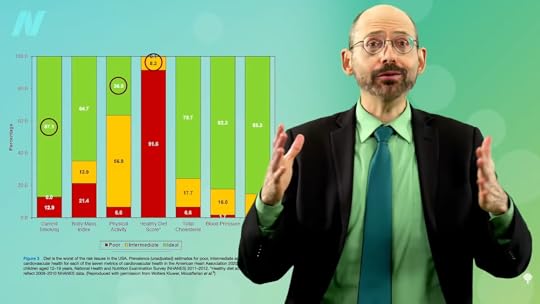
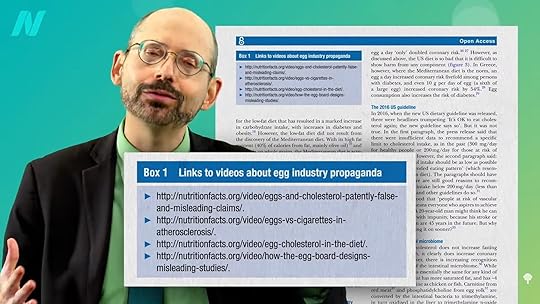
The paper goes on to say, “Box 1 provides links to information about the issue.” I was excited to click on the hyperlink for “Box 1” and was so honored to see four links to my videos on egg industry propaganda, as you can see below and at 1:08 in my video.
The strongest evidence for stroke protection lies in increasing fruit and vegetable intake, with more uncertainty regarding “the role of whole grains, animal products, and dietary patterns,” such as vegetarian diets. One would expect meat-free diets would do great. Meta-analyses have found that vegetarian diets lower cholesterol and blood pressure, as well as enhance weight loss and blood sugar control, and vegan diets may work even better. All the key biomarkers are going in the right direction. Given this, you may be surprised to learn that there hadn’t been any studies on the incidence of stroke in vegetarians and vegans until now. And if you think that is surprising, wait until you hear the results.
“Risks of Ischaemic Heart Disease and Stroke in Meat Eaters, Fish Eaters, and Vegetarians Over 18 Years of Follow-Up: Results from the Prospective EPIC-Oxford Study”: There was less heart disease among vegetarians (by which the researchers meant vegetarians and vegans combined). No surprise. Been there, done that. But there was more stroke, as you can see below, and at 2:14 in my video.

An understandable knee-jerk reaction might be: Wait a second, who did this study? Was there a conflict of interest? This is EPIC-Oxford, world-class researchers whose conflicts of interest may be more likely to read: “I am a member of the Vegan Society.”
What about overadjustment? When the numbers over ten years were crunched, the researchers found 15 strokes for every 1,000 meat eaters, compared to only 9 strokes for every 1,000 vegetarians and vegans, as you can see below and at 2:41 in my video. In that case, how can they say there were more strokes in the vegetarians? This was after adjusting for a variety of factors. The vegetarians were less likely to smoke, for example, so you’d want to cancel that out by adjusting for smoking to effectively compare the stroke risk of nonsmoking vegetarians to nonsmoking meat eaters. If you want to know how a vegetarian diet itself affects stroke rates, you want to cancel out these non-diet-related factors. Sometimes, though, you can overadjust.

The sugar industry does this all the time. This is how it works: Imagine you just got a grant from the soda industry to study the effect of soda on the childhood obesity epidemic. What could you possibly do after putting all the studies together to conclude that there was a “near zero” effect of sugary beverage consumption on body weight? Well, since you know that drinking liquid candy can lead to excess calories that can lead to obesity, if you control for calories, if you control for a factor that’s in the causal chain, effectively only comparing soda drinkers who take in the same number of calories as non-soda-drinkers, then you could undermine the soda-to-obesity effect, and that’s exactly what they did. That introduces “over adjustment bias.” Instead of just controlling for some unrelated factor, you control for an intermediate variable on the cause-and-effect pathway between exposure and outcome.
Overadjustment is how meat and dairy industry-funded researchers have been accused of “obscuring true associations” between saturated fat and cardiovascular disease. We know that saturated fat increases cholesterol, which increases heart disease risk. Therefore, if you control for cholesterol, effectively only comparing saturated fat eaters with the same cholesterol levels as non-saturated-fat eaters, that could undermine the saturated fat-to-heart disease effect.
Let’s get back to the EPIC-Oxford study. Since vegetarian eating lowers blood pressure and a lowered blood pressure leads to less stroke, controlling for blood pressure would be an overadjustment, effectively only comparing vegetarians to meat eaters with the same low blood pressure. That’s not fair, since lower blood pressure is one of the benefits of vegetarian eating, not some unrelated factor like smoking. So, that would undermine the afforded protection. Did the researchers do that? No. They only adjusted for unrelated factors, like education, socioeconomic class, smoking, exercise, and alcohol. That’s what you want. You want to tease out the effects of a vegetarian diet on stroke risk. You want to try to equalize everything else to tease out the effects of just the dietary choice. And, since the meat eaters in the study were an average of ten years older than the vegetarians, you can see how vegetarians could come out worse after adjusting for that. Since stroke risk can increase exponentially with age, you can see how 9 strokes among 1,000 vegetarians in their 40s could be worse than 15 strokes among 1,000 meat-eaters in their 50s.
The fact that vegetarians had greater stroke risk despite their lower blood pressure suggests there’s something about meat-free diets that so increases stroke risk it’s enough to cancel out the blood pressure benefits. But, even if that’s true, you would still want to eat that way. As you can see in the graph below and at 6:16 in my video, stroke is our fifth leading cause of death, whereas heart disease is number one.

So, yes, in the study, there were more cases of stroke in vegetarians, but there were fewer cases of heart disease, as you can see below and at 6:29. If there is something increasing stroke risk in vegetarians, it would be nice to know what it is in hopes of figuring out how to get the best of both worlds. This is the question we will turn to next.

I called it 21 years ago. There’s an old video of me on YouTube where I air my concerns about stroke risk in vegetarians and vegans. (You can tell it’s from 2003 by my cutting-edge use of advanced whiteboard technology and the fact that I still had hair.) The good news is that I think there’s an easy fix.
This is the third in a 12-video series on stroke risk. Links to the others are in the related posts below.
August 8, 2024
Eating to Lower Lp(a)
What should we eat—and not eat—to lower the cardiovascular disease risk factor lipoprotein(a)?
Lipoprotein A, also known as Lp(a), is an independent, genetic, and causal factor for cardiovascular disease and heart attacks. At any level of LDL cholesterol, our risk of heart attack and stroke is two- to three-fold higher when our Lp(a) is elevated. With a high enough Lp(a) level, atherosclerosis continues to progress even if we get our LDL cholesterol way down, which may help explain why so many people continue to have heart attacks and strokes even under treatment for high cholesterol. It’s been suggested that “it would be worthwhile to check Lp(a) levels in a patient who has suffered an event but has no traditional risk factors to explain it.” What’s the point of checking it, though, if there isn’t much we can do about it? “To date, no drug to reduce circulating Lp(a) levels has been approved for clinical use.”
Some researchers blame our lack of knowledge on the fact that Lp(a) is not found in typical lab animals, like rats and mice. It’s only found in two places in nature: primates and hedgehogs. Hedgehogs? How strange is that? No wonder Lp(a) is “an enigmatic protein that has mystified medical scientists ever since” it was first discovered more than half a century ago. But who needs mice when you have men? The level in our bloodstream is “primarily determined” by genetics. For the longest time, Lp(a) was not thought to be significantly influenced by factors such as diet. Given its similarity to LDL, though, one might assume lifestyle changes, “such as increased physical activity or the adoption of a healthy diet,” would help. “However, the effects of these interventions on Lp(a) concentrations are so far either only marginal or lacking in evidence,” but might that be because they have not tried a plant-based diet yet?
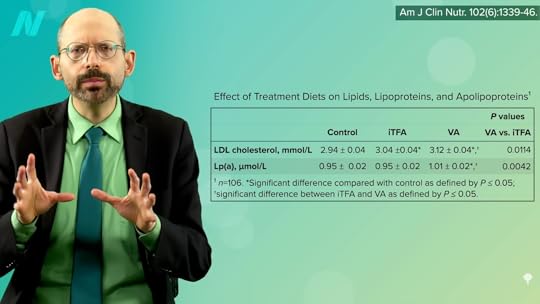
As I discuss in my video How to Lower Lp(a) with Diet, when it comes to raising LDL cholesterol, we’ve known for years that the trans fats found in meat and dairy are just as bad as the industrially produced trans fats found in partially hydrogenated oil and junk food. But, when it comes to Lp(a), as you can see below and at 2:05 in my video, trans fats from meat and dairy appear to be even worse.
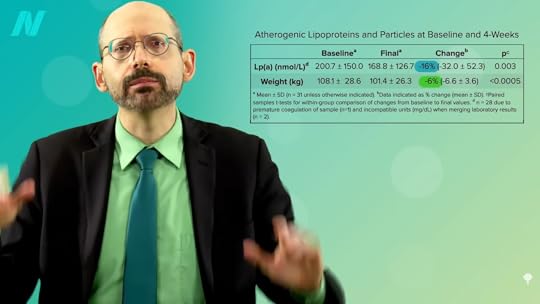
Just cutting out meat and following a lacto-ovo vegetarian diet did not appear to help, but, as you can see below and at 2:19 in my video, when study participants were put on a whole food, plant-based diet packed with a dozen servings of fruits and vegetables a day, their Lp(a) levels dropped by 16 percent within four weeks.

Of course, in those 30 days, the study subjects also lost about 15 pounds, as you can see below and at 2:28, but weight loss does not appear to affect Lp(a) levels, so you figure that it must have been due to the diet.
If you’re already eating a healthy plant-based diet and your Lp(a) levels are still too high, are there any particular foods that can help? As with cholesterol, even if the average total cholesterol of those eating strictly plant-based may be right on target at less than 150, with an LDL under 70, there’s a bell curve with plus or minus 30 points that fall on either side, as you can see below and at 2:45 in my video.

Enter the “Portfolio Diet,” which is not only plant-based, but also adds specific cholesterol-lowing foods—so, think nuts, beans, oatmeal, and berries to drag cholesterol down even further. The infographic is below and at 3:11 in my video.

What about Lp(a)? Nuts have been put to the test. Two and a half ounces of almonds every day dropped levels, but only by about 8 percent. That is better than another nut study, though, that found no effect at all, as you can see below and at 3:29 in my video. An additional study found “no significant changes,” and researchers reported that subjects in their study “did not experience a change in Lp(a).” Ah, nuts.

There is one plant that appears to drop Lp(a) levels by 20 percent, which is enough to take people exceeding the U.S. cut-off down to a more optimum level. And that plant is a fruit: Emblica officinalis, otherwise known as amla or Indian gooseberry. A randomized, double-blind, placebo-controlled study asked smokers before and after the trial about their “mouth hygiene, cough with expectoration, shortness of breath on exertion, loss of appetite, feelings of impending doom, palpitation, sleep deprivation, irritability, heartburn and tiredness,” as well as such objective measurements as their blood count, cholesterol, DNA damage, antioxidant status, and lung function. The amla extract used “showed a significant improvement compared to the placebo group in all the subjective and objective parameters tested with no reports of adverse events.” No side effects at all. That’s unbelievable! No, that’s unbelievable. And indeed, it’s completely not true.
Yes, subjective complaints got better in the amla group, but they got better in the placebo group, too, with arbitrary scoring systems and no statistical analysis whatsoever. And, of the two dozen objective measures, only half could be said to reach any kind of before-and-after statistical significance and only three were significant enough to account for the fact that if you measure two dozen things, a few might pop up as positive if only by chance. Any time you see this kind of spin in the abstract, which is sometimes the only part of a study people read, you should suspect some kind of conflict of interest. However, no conflicts of interest were declared by the researchers, but that’s bullsh*t, as the study was funded by the very company selling those amla supplements! Sigh.
Anyway, one of those three significant findings was the Lp(a), so it might be worth a try in the context of a plant-based diet, which, in addition to helping with weight loss, can dramatically improve blood pressure (even after cutting down on blood pressure medications) and contribute to a 25-point drop in LDL cholesterol. Also, it may contribute to a 30 percent drop in C-reactive protein and significant reductions in other inflammatory markers for “a systemic, cardio-protective effect”—all thanks to this single dietary approach.
You may be interested in my video on Trans Fat in Meat and Dairy. Did you know that animal products are exempted from the ban? See Banning Trans Fat in Processed Foods but Not Animal Fat.
For more on amla and what else it can do, check out the related posts below.
If you missed my previous video on Lp(a), watch Treating High Lp(a)—A Risk Factor for Atherosclerosis.