Michael Greger's Blog, page 8
January 23, 2025
Exploring the Obesity Paradox
How do we explain studies that suggest overweight individuals live longer?
Martin Luther King Jr. warned that human progress is neither automatic nor inevitable, and the same may be true of the human lifespan. In the 1800s, life expectancy was less than 40 years, but it has been “advancing steadily” over the last two centuries, “increasing at approximately 2 years per decade”—until recently. Longevity gains appear “to be faltering or even being reversed.” Thanks to the obesity epidemic, we may now be raising the first generation to live shorter lives than their parents.
“This downward trend in longevity will almost certainly accelerate as the current generation of children—with higher body weights from earlier in life than ever before—reaches adulthood.” Current trends “potentially signal a looming social and economic catastrophe” if the obesity epidemic continues unchecked. In the coming decades, some predict we may lose two to five years or more of life expectancy in the United States. To put that into perspective, a miracle cure for all forms of cancer would only add three and a half years to the average U.S. life expectancy. In other words, reversing the obesity epidemic might save more lives than curing cancer.
The evidence that being overweight increases our risk for debilitating diseases like diabetes is considered “indisputable.” However, surprisingly, there is controversy surrounding body weight and overall mortality. In 2013, scientists with the Centers for Disease Control and Prevention (CDC) published a meta-analysis in the Journal of the American Medical Association suggesting that being overweight was advantageous. Grades 2 and 3 obesity, such as being an average height of 5’6″ and weighing about 216 pounds (98 kg) or more, were associated with living a shorter life, but grade 1 obesity, weighing about 185 to 215 pounds (84 to 97 kg) at that height, was not. Being overweight (about 155 to 185 pounds/70 to 83 kg at 5’6″) appeared to be protective compared to those who were a “normal weight” of 115 to 155 pounds (52 to 69 kg). The overweight individuals, those with a body mass index (BMI) of 25 to 30, appeared to live the longest.
Headline writers were giddy. “Being overweight can extend your life rather than shorten it,” read one. “Dreading your diet? Don’t worry—plump people live LONGER than their skinnier counterparts…” read another. “Extra pounds mean a lower chance of death.” Not surprisingly, the study ignited a firestorm of controversy in the public health community. The study was called “ludicrous,” “flawed,” and “misleading.” The chair of nutrition at Harvard lost his cool, calling the study “really a pile of rubbish” and fearing the food industry might exploit the study in the same way the petroleum industry misuses “controversy” over climate change.
Public health advocates can’t just dismiss data they find inconvenient, though. Science is science. But how could being overweight increase the risk of life-threatening diseases, yet, at the same time, make you live longer? This became known as “The Obesity Paradox,” the subject of my video Is the Obesity Paradox Real or a Myth?.
The solution to the puzzle appears to lie with two major sources of bias, the first being “confounding by smoking.” The nicotine in tobacco can lead to weight loss. So, if you’re skinnier because you smoke, then no wonder you’d live a shorter life, albeit with a slimmer waist. The failure to control for the effect of smoking in studies purporting to show an “obesity paradox” leads to the dangers of obesity being “grossly underestimated.”
The second major source of bias is reverse causality. Instead of lower weight leading to life-threatening diseases, isn’t it more likely that life-threatening diseases lead to lower weight? Conditions such as hidden tumors, chronic heart or lung disease, alcoholism, and depression can all cause unintentional weight loss for months or even years before they are even diagnosed. It’s normal to be overweight in the United States, for example. So, people who are “abnormally” thin—in other words, at an ideal weight—may be taking care of themselves, but they may instead be “heavy smokers, frail and elderly, and seriously ill with weight loss due to their disease…”
To put the obesity paradox to the test once and for all, The Global BMI Mortality Collaboration was formed, reviewing data from more than 10 million people from hundreds of studies in dozens of countries—the largest evaluation of BMI and mortality in history. To help eliminate bias, the researchers omitted smokers and those with known chronic disease, then excluded the first five years of follow-up to try to remove from the analysis those with undiagnosed conditions who lost weight due to an impending death. And? The results were clear: “This analysis has shown that both overweight and obesity (all grades) were associated with increased all-cause mortality”—a greater risk of dying prematurely. So, “adjusting for these biases leads to eliminating the obesity paradox.” In other words, the so-called obesity paradox appears to be “just a myth.”
Indeed, when intentional weight loss is put to the test, people live longer. There are bariatric surgery studies like the SOS trial that show that weight loss reduces long-term mortality, and randomizing study participants to weight loss through lifestyle changes shows the same thing. Losing a dozen pounds through diet and exercise was found to be associated with a 15 percent drop in overall mortality. Now, exercise alone may extend lifespan even without weight loss, but there appears to be a similar longevity benefit of weight loss through dietary means alone.
If you missed the previous blog posts in my series on the ABCs of obesity, see:
The Best Knee Replacement Alternative for Osteoarthritis Treatment The Effects of Obesity on Back Pain, Blood Pressure, Cancer, and Diabetes The Effects of Obesity on Dementia, Brain Function, and Fertility The Effects of Obesity on Gallstones, Acid Reflux, and Cardiovascular Disease The Effects of Obesity on the Immune System and Kidney and Liver DiseasesCheck out the final two videos in this series: What’s the Ideal BMI? and What’s the Ideal Waist Size?.
I cover all of this and more at length in my book How Not to Diet, and its companion, The How Not to Diet Cookbook, has more than 100 delicious Green-Light recipes that incorporate some of my 21 Tweaks for the acceleration of body fat loss.
Why are people obese in the first place? I have a whole series of videos on that topic. Check the videos in the related posts.
January 21, 2025
Obesity’s Impacts on Our Immune System and Kidney and Liver Diseases
What are the effects of weight loss on natural killer cell function, our first line of immune defense against cancer, kidney function, and fatty liver disease?
In the ABCs of the health consequences of obesity, I is for Immunity.
The SOS trial followed the fates of thousands of bariatric surgery patients for a decade or two, compared to a control group who maintained their weight. Those who surgically lost about 20 percent of their body weight not only lived longer, thanks in part to less diabetes and less cardiovascular disease, but they also got less cancer. This may be because anti-tumor immunity appears to be affected by weight.
Natural killer cells are our immune system’s first line of defense against cancer cells and many viral infections, “and their function is severely impaired in individuals with obesity.” When individuals who were obese were randomized to a weight-loss program, researchers found a significant reactivation of the participants’ natural killer cell function within just three months. The program involved an exercise component, though, so it’s hard to tease out the impact of the weight loss itself since physical activity on its own can boost natural killer cell activity.
On the other end of the immune spectrum, obesity is suspected to be a causal risk factor for the development of the autoimmune disease multiple sclerosis. This suggests obesity is associated with the worst of both worlds when it comes to immune function: underactivity when it comes to protecting against cancer and infection, and overactivity when it comes to certain inflammatory autoimmune conditions.
J is for Jaundice. Thanks to the obesity epidemic, nonalcoholic fatty liver disease is now the most common liver disorder in the industrialized world. Fat doesn’t just end up in our belly and thighs but inside some of our internal organs. More than 80 percent of individuals with abdominal obesity may have fatty infiltration into their liver, and in those with severe obesity, the prevalence can exceed 90 percent. This can lead to inflammation, scarring, and, ultimately, cirrhosis and liver cancer, as you can see below and a 2:10 in my video The Effects of Obesity on the Immune System and Kidney and Liver Diseases. Currently, this nonalcoholic fatty hepatitis is the leading cause of liver transplants in American women.

K is for Kidneys. Obesity is also “one of the strongest risk factors for new-onset chronic kidney disease.” Our kidneys compensate for the metabolic demands of excess weight by red-lining into what’s called “hyperfiltration” to deal with the extra workload. This resulting increased pressure within our kidneys can damage the sensitive structures and increase the risk of kidney failure over the long term.
What about L, M, N, O, P through Z? If you want to continue through the alphabet, L could be for diminished lung function, M could be for metabolic syndrome, and so on. There is even an X—for xiphodynia—pain at the tip of the bottom of the breastbone from being bent forward by an expanding abdomen.
Given the myriad health conditions associated with excess weight, “annual medical spending attributable to an obese individual” is nearly $2,000 per year and workers who are obese with multiple conditions can cost companies up to $10,000 more in healthcare coverage compared to “their lean counterpart.” This may account for some of the wage gap that employees who are obese may experience, as companies try to pass along these costs of “their higher health insurance premiums,” beyond just brazen discrimination. Between healthcare costs and diminished productivity in terms of lost workdays, the total lifetime costs of obesity for children and teens have been estimated to exceed $150,000.
Some estimates peg the annual “medical care costs of obesity in the United States” at about $150 billion, with another $50 billion per year added by 2030 as our increasingly heavy Baby Boomers continue to age. Others diametrically disagree, based on the morbid fact that individuals who are obese may not live as long. Just as “the high medical costs of smoking-related diseases are more than offset by lower survival of smokers,” the lifetime healthcare costs of individuals who are obese may turn out to be lower because they are expected to die so much sooner. So, the true cost may be more in lives, rather than dollars. How much does being overweight cut your life short? I’ll explore just that question next.
If you missed the previous blog posts in my series on the ABCs of obesity, see related posts below.
I continue the topic of obesity and weight with these videos: Is the Obesity Paradox Real or a Myth? and Friday Favorites: What’s the Ideal BMI and Waist Size?.
For more on the health conditions discussed in this video, see the immune function, kidney disease, and liver health topic pages.
January 16, 2025
Obesity’s Impacts on Gallstones, Acid Reflux, and Heart Disease
Sufficient, sustained weight loss may cut the risk of fatal heart attacks and strokes in half.
In the ABCs of health consequences of obesity, G is for Gallstones.
The top digestive reason people are hospitalized is a gallbladder attack. Every year, more than a million Americans are diagnosed with gallstones, and about 700,000 must have their gallbladders surgically removed. It is a relatively safe procedure, with complication rates tending to be under 5 percent and a mortality rate of only about 1 in 1,000. However one in ten may develop a post-cholecystectomy syndrome of persistent gastrointestinal symptoms long after their gallbladder is removed.
What are gallstones made of? In 80 to 90 percent of cases, gallstones are mostly crystalized cholesterol, forming like rock candy in our gallbladder when cholesterol gets too concentrated. This was used to explain why some small, early studies found that non-vegetarians had a higher incidence of gallstones. However, results from more recent, larger studies are more equivocal; one study suggests that a “vegetarian diet may therefore protect” against gallbladder disease, for instance, while another shows higher rates among vegetarians, independent of weight.
As I discuss in my video The Effects of Obesity on Gallstones, Acid Reflux, and Cardiovascular Disease, the biggest purported cause-and-effect risk factor may be obesity, increasing risk as much as sevenfold, as you can see below and at 1:32 in my video, with a doubling of risk even at the heavier side of “the normal BMI range.”
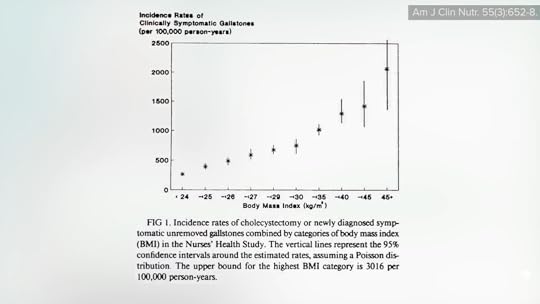
Ironically, rapid weight loss may also be a trigger. Half a pound (1.5 kg) a day has been deemed the upper limit for medically safe weight loss, based on gallstone formation. Ultrasound studies found that, above that, the chance of new gallstones can go from less than 1 in 200 a week to closer to 1 in 40, as shown below and at 1:59.
To help prevent a gallstone attack, we can increase our fiber intake. Not only is dietary fiber intake associated with less gallbladder disease in the first place, but those placed on high-fiber foods during a weight-loss regimen suffered significantly less gallbladder sludging than those losing the same amount of weight without getting the extra fiber.
G is also for gastroesophageal reflux disease, or GERD. Fiber-rich food consumption decreases the risk of acid reflux, too. I previously explored how chronically straining at stool may push part of the stomach up into the chest cavity. Well, excess abdominal pressure due to obesity may have the same effect, pushing acid up into the throat and causing heartburn and inflammation. The increased pressure on the abdominal organs associated with obesity may also explain why overweight women suffer from more vaginal prolapse, where organs such as the rectum push out and into the vaginal cavity.
The deadliest letter in the alphabet of obesity consequences is H, which is for Heart Disease. Of the four million deaths attributed to excess body weight every year around the world, nearly 70 percent are due to cardiovascular disease. Is it just because of eating poorly? Mendelian randomization studies suggest that people randomized from conception to be heavier—based only on genetics—do indeed have higher rates of heart disease and stroke regardless of what they eat. The question is: If you lose weight, does your risk drop?
Enter the Swedish Obese Subjects (SOS) trial, the first long-term controlled trial to compare the outcomes of thousands of bariatric surgery patients to matched control subjects who started out at the same weight but went the nonsurgical route. Individuals in the control group maintained their weight, whereas those in the surgical group maintained about a 20 percent weight loss over the next 10 to 20 years. In that period, those in the weight-loss group not only developed 80 percent less diabetes, but they suffered significantly fewer heart attacks and strokes. So, unsurprisingly, they significantly reduced their total mortality overall. Ten years out, the weight-loss group appeared to cut their risk of fatal heart attacks and strokes in half, as shown below and at 4:23 in my video.

If you missed the previous videos in my series on the ABCs of obesity, see:
The Best Knee Replacement Alternative for Osteoarthritis Treatment The Effects of Obesity on Back Pain, Blood Pressure, Cancer, and Diabetes The Effects of Obesity on Dementia, Brain Function, and FertilityI continue the topic of obesity and weight with videos in the related posts below.
For more on the health conditions discussed in this video, see the gallstones, GERD, and heart disease topic pages.
The GERD-related video I mentioned is Diet and Hiatal Hernia.
January 14, 2025
Obesity’s Impacts on Our Brain, Dementia, and Fertility
Weight loss can decrease dementia risk and improve mental performance and fertility.
As I’ve discussed previously, in the ABCs of the health consequences of obesity, A is for Arthritis, B is for Back Pain and Blood Pressure, C is for Cancer, and D is for Diabetes. That brings us to E, which is for Encephalopathy.
Encephalopathy means brain disease. There are consistent data linking obesity in middle age to a higher risk of dementia later in life. Researchers found that individuals who are overweight have about a one-third higher risk of dementia and those who are obese in mid-life have about 90 percent greater risk. The risk isn’t limited only to future dysfunction, though. People with excess body weight don’t appear to think as clearly at any age.
“It was found that obese participants showed broad impairments on executive functions” of the brain, including working memory, decision-making, planning, cognitive flexibility, and verbal fluency. “From resisting temptation to keeping long-term goals in mind, executive functions play a critical role in everyday life,” noted a meta-analysis and review of 72 studies on the issue.
According to researchers, people may think about their obesity and the resulting stigma they experience as much as five times an hour, but the cognitive deficits do not appear to arise just from distraction; there are structural brain differences between individuals who are at an ideal weight versus overweight.
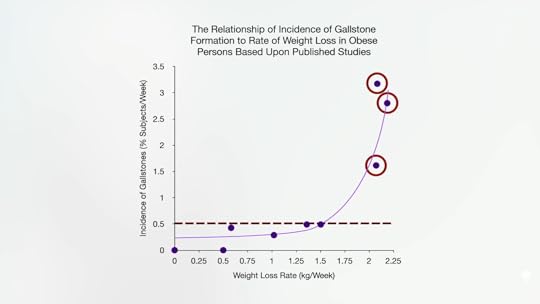
A review entitled “Does the Brain Shrink as the Waist Expands?” noted gray matter atrophy across all ages among those carrying excess body fat. It’s this reduced brain volume that has been correlated with lower executive function. As you can see below and at 1:42 in my video The Effects of Obesity on Dementia, Brain Function, and Fertility, compromised integrity of the rest of the brain—the white matter—suggests accelerated brain aging, even in young adults and children with obesity.
Cognitive deficits in younger populations suggest there’s something about obesity itself that is affecting brain function, rather than a later clinical consequence, such as high blood pressure. Purported mechanisms for this executive dysfunction include obesity-related inflammation and oxidative stress.
So, does weight loss improve cognitive function? Based on a meta-analysis of 20 studies, researchers found that mental performance across a variety of domains can be significantly improved with even modest weight loss. However, no studies have yet to be done to determine if this then translates into a normalization of Alzheimer’s disease risk.
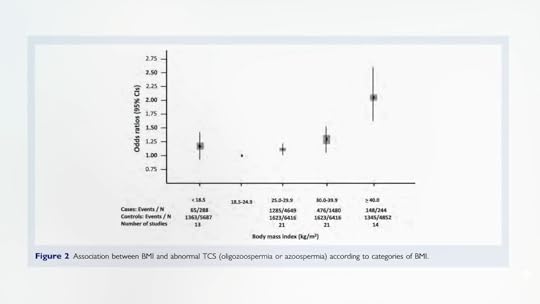
Back to the ABCs of obesity’s health consequences, F is for Fertility—or rather failed fertility. “Overweight and obese persons seeking fertility should be educated on the detrimental effects of fatness and the benefits of weight reduction, including improvement in pregnancy rates,” one meta-analysis concluded. Men also may suffer impaired fertility. The heavier a man is, the greater his risk of having a low sperm count or being completely sterile, as you can see below and at 3:01 in my video. This may be due in part to the effects of excess body fat on testosterone levels.
Fat isn’t the primary site of estrogen production in only postmenopausal women, but in men, too. An enzyme in body fat converts testosterone into estrogen. Men losing weight and going from obese to overweight could potentially raise the testosterone levels in their blood by 13 percent.
A more dramatic cause of infertility in obese men is called a “hidden penis.” The condition, which is also described in the medical literature as a “hidden, buried, concealed, trapped, and inconspicuous” penis, occurs when excess fat in the pubic area subsumes the penis (since its base is attached internally to the pubic bone). The moist enfolding skin surfaces can result in chronic inflammatory dermatitis leading to scarring and requiring a surgical intervention.
If you missed the previous blog posts, I covered The Best Knee Replacement Alternative for Osteoarthritis Treatment and The Effects of Obesity on Back Pain, Blood Pressure, Cancer, and Diabetes.
I continue the topic of obesity and weight with videos in the related posts below.
I cover all of this and more at length in my book How Not to Diet, and its culinary companion, The How Not to Diet Cookbook, has more than 100 delicious, weight-conscious recipes. Request them from your local library.
For more on the health conditions discussed in this video, see the Alzheimer’s disease, cognition, and fertility topic pages.
January 9, 2025
Obesity’s Impact on Back Pain, Blood Pressure, Cancer, and Diabetes
Losing weight can reduce sciatica, hypertension, and cancer risk, as well as reverse type 2 diabetes.
In the ABCs of the health consequences of obesity, A is for Arthritis, as I discussed in my previous blog post, and B is for Back Pain. Being overweight is not just a risk factor for low back pain, but it is also a risk factor for sciatica (a radiating nerve pain), as well as degenerating lumbar discs and disc herniation. Similar to what we learned in the arthritis story, this may also be due to a combination of the excess weight, high cholesterol, and inflammation associated with being overweight. Why cholesterol? Studies of autopsies and angiographies show that the lumbar arteries that feed our spine can get clogged with atherosclerosis and starve the disks in our lower back, as you can see below and at 0:47 in my video The Effects of Obesity on Back Pain, Blood Pressure, Cancer, and Diabetes.

B is also for Blood Pressure. Excess visceral fat—for example, internal abdominal fat—can physically compress our kidneys. The increased pressure can effectively squeeze sodium back into our bloodstream, increasing our blood pressure. Together, the combination of obesity and hypertension can have “disastrous health implications,” but the good news is that just a few pounds of weight loss can help take off the pressure. Losing excess weight has been described as “a vital strategy for controlling hypertension.” In fact, researchers found that losing around nine pounds (4 kg) may lower blood pressure about as much as cutting salt intake approximately in half can.
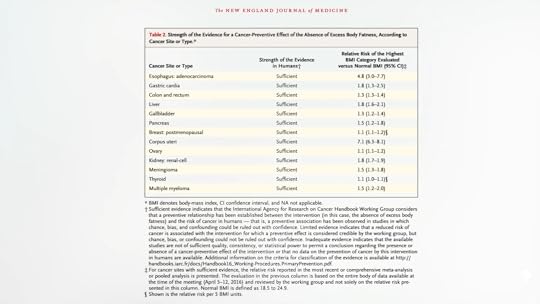
C is for Cancer. As many as three-quarters of people surveyed “were unaware that being overweight or obese increased a person’s risk of cancer,” when, in fact, based on a comprehensive review of more than a thousand studies, excess body fat raises the risk of most cancers, including esophageal, stomach, colorectal, liver, gallbladder, pancreatic, breast, uterine, ovarian, kidney, brain, thyroid, and bone marrow (multiple myeloma) cancers, as you can see below and at 2:00 in my video.
It could be the chronic inflammation of obesity or perhaps it is the high insulin levels due to insulin resistance. (Besides controlling blood sugars, insulin is also “a potent growth factor” that can promote tumor growth.) In women, it could also be the excess estrogen.
After the ovaries shut down at menopause, fat takes over as the principal site of estrogen production. That’s why women who are obese have up to nearly twice the estrogen levels circulating in their bloodstream, which is associated with an increased risk of developing breast cancer and dying from it. The data on prostate cancer aren’t as strong, though obesity is associated with increased risk of invasive penis cancer.
One of the reasons we’re confident the link between obesity and cancer is cause-and-effect—and not just an indirect consequence of eating poorly—is that the overall risk of cancer goes down when people lose weight, even through bariatric surgery. Researchers found that those experiencing a sustained weight loss of about 40 pounds (19.9 kg) after surgery went on to develop around one-third fewer cancers over the subsequent decade, compared with matched individuals in the nonsurgical control group who continued to slowly gain weight over time. The exception, though, is colorectal cancer.
“Colorectal cancer is the only known malignancy where the risk of being diagnosed with disease seems to increase after obesity surgery.” Indeed, after bariatric surgery, the rate of rectal cancer death may triple. The rearrangement of anatomy involved in one of the most common surgeries—Roux-en-Y gastric bypass—is thought to increase bile acid exposure along the intestinal lining. This causes sustained pro-inflammatory changes even years after the procedure, which is thought responsible for the increased cancer risk. In contrast, losing weight by dietary means has the potential to decrease obesity-related cancer risk across the board.
D is for Diabetes. As presented in a consensus statement from the International Diabetes Federation, obesity is considered the single most important risk factor for the development of type 2 diabetes, which is the leading cause of kidney failure, lower-limb amputations, and adult-onset blindness. Ironically, many of the leading drugs used to treat diabetes (including insulin itself) cause further weight gain, creating a vicious cycle.
So, again, using lifestyle medicine to treat the underlying cause is not only safer, simpler, and cheaper, but can also be most effective.
If you missed my previous video, check out The Best Knee Replacement Alternative for Osteoarthritis Treatment.
Coming up next? See related posts below.
I continue the topic of weight control with these videos that may be of interest to you: Is the Obesity Paradox Real or a Myth? and Friday Favorites: What’s the Ideal BMI and Waist Size?.
For more on back pain, blood pressure, cancer, and diabetes, check out their topic pages.
January 7, 2025
Top 10 NutritionFacts.org Videos of 2024
We create more than a hundred new videos every year. They are the culmination of countless hours of researching, writing, editing, animating, and producing. We comb through thousands of scientific papers from the peer-reviewed medical literature so busy people like you don’t have to!
In 2024, I covered a wide variety of hot topics. I released an update on why I changed my mind on water fluoridation, a series on the benefits and side effects of flu, pneumonia, and shingles vaccines, and, of course, a lot on aging and anti-aging based on my research for How Not to Age. Which videos floated to the top last year?
#10 Benefits and Side Effects of the Flu Vaccine
 Randomized placebo-controlled trials show that flu shots can be extraordinary lifesavers. Can you prevent the flu with foods and supplements, like elderberry and echinacea? See Elderberry Benefits and Side Effects: Does It Help with Colds and the Flu?.
Randomized placebo-controlled trials show that flu shots can be extraordinary lifesavers. Can you prevent the flu with foods and supplements, like elderberry and echinacea? See Elderberry Benefits and Side Effects: Does It Help with Colds and the Flu?.
#9 The Pros and Cons of Testing PSA Levels for Prostate Cancer
 Given the clear harms and the small and uncertain benefits of PSA testing, most men would presumably decide to decline to undergo it if they knew all the facts, but that’s up to each individual to decide. If you do get diagnosed with prostate cancer, what can you do with your diet, in addition to any other therapies you might choose? See the Prostate Cancer topic page for all related videos.
Given the clear harms and the small and uncertain benefits of PSA testing, most men would presumably decide to decline to undergo it if they knew all the facts, but that’s up to each individual to decide. If you do get diagnosed with prostate cancer, what can you do with your diet, in addition to any other therapies you might choose? See the Prostate Cancer topic page for all related videos.
Five massive new trials have been published recently, randomizing tens of thousands to various formulations of fish oil versus placebo. Want to know my omega-3 recommendations? See my Optimum Nutrient Recommendations.
#7 The Best Dietary Detox
 By eating at a lower rung on the food chain, those choosing plant-based diets aren’t as exposed to the industrial pollutants that bioaccumulate up the ladder.
By eating at a lower rung on the food chain, those choosing plant-based diets aren’t as exposed to the industrial pollutants that bioaccumulate up the ladder.
#6 How to Lower Lp(a) with Diet
 What should we eat and what should we avoid to lower the cardiovascular disease risk factor lipoprotein(a)?
What should we eat and what should we avoid to lower the cardiovascular disease risk factor lipoprotein(a)?
#5 Why Do Milk Drinkers Live Shorter Lives on Average?
 How might we reduce the risk of premature death from dairy consumption? One way is to switch to soy milk. Check out Is Soy Milk the Most Nutritious Non-Dairy Milk?.
How might we reduce the risk of premature death from dairy consumption? One way is to switch to soy milk. Check out Is Soy Milk the Most Nutritious Non-Dairy Milk?.
#4 How to Boost Your Endothelial Progenitor Cells (EPCs) for Heart Health
 How can we improve the capacity of our blood vessels to repair themselves? We can boost the ability of our endothelium to function by eating nitrate-rich vegetables, like beets and greens. See Oxygenating Blood with Nitrate-Rich Vegetables.
How can we improve the capacity of our blood vessels to repair themselves? We can boost the ability of our endothelium to function by eating nitrate-rich vegetables, like beets and greens. See Oxygenating Blood with Nitrate-Rich Vegetables.
#3 Preventing and Treating Osteoporosis (Webinar Recording)
 In this two-hour webinar, I cover bone mineral density screening, common over-the-counter drugs like acid blockers that may increase fracture risk, how safe and effective the current oral and injected osteoporosis medications are, which foods may help protect our bones, the best type and frequency of exercise, and how to reduce fall risk.
In this two-hour webinar, I cover bone mineral density screening, common over-the-counter drugs like acid blockers that may increase fracture risk, how safe and effective the current oral and injected osteoporosis medications are, which foods may help protect our bones, the best type and frequency of exercise, and how to reduce fall risk.
#2 How Not to Age – Live Presentation
 In this live lecture, I cover highlights from my book, How Not to Age, which became a New York Times Best Seller. I hope it helps with your New Year’s resolutions. As always, all proceeds I receive from all of my books are donated directly to charity.
In this live lecture, I cover highlights from my book, How Not to Age, which became a New York Times Best Seller. I hope it helps with your New Year’s resolutions. As always, all proceeds I receive from all of my books are donated directly to charity.
#1 Can Alzheimer’s Disease Be Reversed with a Plant-Based Diet?
 Dr. Dean Ornish published the first randomized controlled trial investigating whether a plant-based diet and lifestyle program may reverse the course of early-stage Alzheimer’s disease. What does improving the cognition and function of Alzheimer’s patients with lifestyle medicine actually translate into in terms of human impact? Check out A Testimonial from Dr. Ornish’s Alzheimer’s Progression Reversal Study.
Dr. Dean Ornish published the first randomized controlled trial investigating whether a plant-based diet and lifestyle program may reverse the course of early-stage Alzheimer’s disease. What does improving the cognition and function of Alzheimer’s patients with lifestyle medicine actually translate into in terms of human impact? Check out A Testimonial from Dr. Ornish’s Alzheimer’s Progression Reversal Study.
Thank you for being a part of this community. We gained more than 140,000 new subscribers on YouTube in 2024, and the number of people we can reach with this life-saving, life-changing information continues to grow.
January 2, 2025
The Best Alternative to Knee Replacement for Osteoarthritis
Is there a non-surgical alternative to knee replacement surgery that treats the cause and offers only beneficial side effects?
The largest study in history on the health effects of being overweight, analyzing data from more than 50 million people from nearly 200 countries, found that excess body weight accounts for the premature deaths of about four million people every year. Most of these deaths are from heart disease, but the researchers “found convincing or probable evidence” linking obesity to 20 different disorders—a veritable alphabet soup of potential health concerns.
In the ABCs of the health consequences of obesity, A is for arthritis. Obesity can make rheumatoid arthritis worse and increase the risk of another inflammatory joint disease—gout, the so-called disease of kings. The most common joint disease in the world, though, is osteoarthritis, and obesity may be its “main modifiable risk factor.”
Osteoarthritis develops when the cartilage that lines and cushions our joints breaks down faster than our body can build it back up. Our knee is the most commonly affected joint, leading to the assumption that the association with obesity was simply due to the excess wear and tear from the added load on the joints. But non-weight-bearing joints, like our hands and wrists, can also be affected, suggesting the link isn’t “purely mechanical.” Obesity-related dyslipidemia may play a role, with elevations in the amounts of triglycerides, fat, and cholesterol in the blood aggravating inflammation in the joints, just like cholesterol can exacerbate the inflammation in our artery walls.
Osteoarthritis sufferers not only have higher cholesterol levels in the blood, but they also have them within their joints, as you can see below and at 1:52 in my video The Best Knee Replacement Alternative for Osteoarthritis Treatment, in aspirated joint fluid and also found in the cartilage itself.
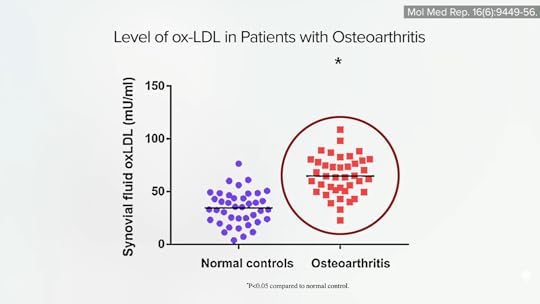
When cholesterol is dripped onto human cartilage in a petri dish, the inflammatory degeneration worsens, which helps explain why the higher our cholesterol, the worse our disease, as shown below and at 2:05.

Cholesterol-lowering statin drugs may help prevent and also treat osteoarthritis, as can a cholesterol-lowering diet. In fact, a healthy enough plant-based diet may offer the best of both worlds, dropping cholesterol as much as a starting dose of a statin drug—within a single week—and having only good side effects, such as lowering blood pressure and facilitating weight loss.
Even losing only about a pound a year for a decade may decrease the odds of developing osteoarthritis by more than 50 percent. Weight reduction may even obviate the need for knee replacement surgery. Osteoarthritis sufferers with obesity who were randomized to lose weight improved their knee function as much as those undergoing surgery—and did so within just eight weeks. The researchers concluded that losing 20 pounds of fat “might be regarded as an alternative to knee replacement.”
Isn’t it easier to get your knees replaced than lose 20 pounds, though? Rarely discussed is the fact that nearly 1 in 200 knee replacement patients lose their lives within 90 days of surgery. Given the extreme popularity of this surgery—about 700,000 are performed each year in the United States—an orthopedics journal editor suggested that “people considering this operation are inadequately attuned to the possibility that it may kill them.” Arguably, that’s the single most salient fact to share with a patient who is considering the operation. Responding to the question of whether patients should be told about the chance the operation may kill them, an orthopedic surgeon said: “To me, the real question is whether this knowledge will help the patient. Will it add to the anxiety of the already anxious patient, perhaps to the point of denying that patient a helpful operation? Or will this knowledge motivate a less-handicapped patient to stick to a diet and physical activity regime? Ultimately, then, the question boils down to the surgeon’s judgment.”
Even among the vast majority who survive the surgery, approximately one in five knee replacement patients describe being unsatisfied with the outcome. Weight loss with a healthy diet, on the other hand, may offer a nonsurgical alternative that treats the cause and has only beneficial side effects.
I continue the alphabet of obesity with the next few videos in the related posts below.
You may be interested in my book on weight loss, How Not to Diet, and its companion, The How Not to Diet Cookbook, which is full of health-promoting, Green-Light recipes. Request them from your local library.
For more on joint health, visit the topic page.
December 31, 2024
Does Fasting Help Autoimmune Diseases?
Various fasting regimens have been attempted for inflammatory autoimmune diseases, such as lupus, ankylosing spondylitis, chronic urticaria, mixed connective-tissue disease, glomerulonephritis, and multiple sclerosis, as well as osteoarthritis and fibromyalgia.
The strongest evidence of the benefits of fasting surrounds the treatment of rheumatoid arthritis, an autoimmune joint disease, as I detailed in my previous blog post. A German study suggested benefits for osteoarthritis, too, and reported improvements in pain and joint function, but we’d really need randomized controlled studies to know for sure. The researchers despaired they only had 30 patients, but that’s 30 times more than many reports on fasting in the medical literature, which may detail only single cases.
One woman, for example, with a rare autoimmune disease known as mixed connective-tissue disease, which can cause all sorts of painful and distressing symptoms, was treated with steroids in an attempt to suppress her immune system. After 21 days of fasting, and off her medications, “she had no further complaints.” More importantly, her symptoms seemed to stay away, and “she remained free of medication.” So, does fasting work for mixed connective tissue disease? All we can say is that it worked at least once.
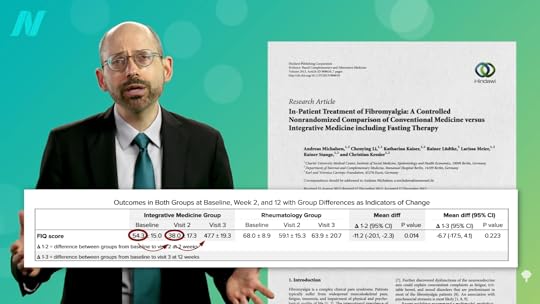
A similar success story was reported with fibromyalgia. A woman with pain throughout her body, who couldn’t sustain activity and was on a lot of drugs, became “symptom-free” after a 24-day fast and remained that way at her “follow-up visit 1 month later.” However, when a modified fasting regimen was tried on dozens of individuals, the benefits seen at week 2 largely disappeared by week 12, as shown below and at 1:32 in my video Fasting for Autoimmune Diseases.
What about lupus? A 45-year-old woman who had remained in pain despite taking immunosuppressive drugs was pain-free by day four of fasting and remained symptom-free for one year when her symptoms began to recur, but she wiped them out again with a second seven-day fast, “after which she had no symptoms.” Note, though, that she didn’t only fast. She water-only fasted, then followed it with a plant-based diet in an attempt to solidify the gains. On its own, a strictly plant-based diet without any animal protein has been shown to control symptoms in at least some cases.
The same with sacroiliitis, a common manifestation of ankylosing spondylitis, an autoimmune arthritis that primarily affects the spine, causing back pain that can last for years. In the case of a 33-year-old man, all sorts of conventional therapies and drugs were tried, but the pain wouldn’t go away. So, the complete avoidance of animal foods was recommended, and “the complaints improved distinctly and persistently” within days—until the patient ate meat again. Once again, back on plant-based nutrition, he was off most of his drugs and almost completely free of symptoms. So, at least in this case, inflammatory pain refractory to other treatments was abolished by eating more healthfully. At least it’s worth a try!
Autoimmune glomerulonephritis, where your body attacks your own kidneys, is a common manifestation of lupus. In a case series, 29 patients were fasted for 60 hours, then had only fruits and vegetables until they got better. They described such remarkable recoveries that fasting, in their opinion, “should be an essential part of treatment.”
What about multiple sclerosis, an autoimmune nerve disease? Individuals with MS were randomized to a “fasting-mimicking diet”—in this case, a modified fast that started out with an 800-calorie-a-day diet of fruit, rice, or potatoes, followed by a week sipping a few hundred calories of flaxseed oil and vegetable broth, then transitioning to a plant-based Mediterranean diet. Over the next three months, they experienced a significant improvement in overall quality of life. They also tried a ketogenic diet, but that failed to offer clinically or statistically significant overall benefit, as you can see below and at 3:34 in my video.

And, finally, let’s look at chronic urticaria (hives), where you get a rash of itchy weals and welts, as seen here and at 3:40 in my video. Individuals started to improve on day 3 of the fast, and their hives completely disappeared by day 11. This is consistent with studies from Germany and Japan that evidently showed around 75 percent effectiveness for such patients with what looks like some sort of tea with sugar diet. It’s certainly worth giving fasting therapy a try, but, of course, fasting should only be done under trained medical supervision. Otherwise, you’d never know if you have some hidden underlying kidney issue that could land you in a coma, then maybe in the morgue. You have to have your kidney function and electrolytes monitored to make sure your body is up for the challenge.

“Despite the possible good outcomes, water-only fasting is not a cure or treatment in the traditional sense; it is simply intended to promote the body’s self-healing mechanisms.” Since fasting is unsustainable, by definition, “to maintain the results obtained by water-only fasting, it is necessary to adhere to a health-promoting lifestyle that includes a diet of minimally processed plant foods, adequate sleep, and robust physical exercise.”
If you haven’t seen it yet, check out my related video Fasting for Rheumatoid Arthritis.
I’ve held three webinars on fasting. All of the videos are available for free on NutritionFacts.org, but you can also get them in a digital download—as a bundle or separately. See:
Intermittent Fasting Fasting for Disease Reversal Fasting and CancerTo see all of the fasting videos currently on the site, please visit our fasting topic page.
Interested in more on using diet to prevent and treat autoimmune diseases? Check out the related posts below.
December 26, 2024
Does Fasting Help Rheumatoid Arthritis?
Fasting, followed by a plant-based diet, is put to the test for autoimmune inflammatory joint disease.
Alan Goldhamer is the founder of the TrueNorth Health Center in Santa Rosa, California, where 10,000 individuals have fasted for “a variety of conditions from diabetes and cardiovascular disease to autoimmune diseases.” He noted that “conditions that seemed to be tied to dietary excess tended to respond predictably to the use of fasting followed by a health-promoting diet,” which he describes as one that is “low salt, vegan, high fiber, low fat, low protein, and low sugar.”
“This approach offers people an option to make lifestyle changes, eliminate the cause of the problem, and stabilize their conditions, to the point where the medication is no longer needed.” It’s in contrast to “conventional medicine, which is more about the suppression of the symptoms associated with the disease, rather than removing the underlying mechanisms by which they are caused.”
Said Dr. Goldhamer: “If you treat high blood pressure medically, they tell you, ‘You must take these drugs the rest of your life.’ If you have diabetes, they’ll tell you, ‘You’ll be on these medications the rest of your life.’ If you have autoimmune disease, like lupus, rheumatoid arthritis, ulcerative colitis, ankylosing spondylitis, psoriasis, or eczema, you will be told, ‘You must be on medications the rest of your life,’ because medicine guarantees you will never recover. They promise you, if you follow their advice explicitly, you will be sick the rest of your life.”
Preliminary data suggest that fasting may benefit “metabolic diseases, pain syndromes, hypertension [high blood pressure], chronic inflammatory diseases, atopic [allergic] diseases, and psychosomatic disorders,” but the highest level of evidence we have for the benefits of fasting are in regard to rheumatic diseases—autoimmune inflammatory joint diseases, like rheumatoid arthritis.
Nearly a century ago, it was written that “diet treatment is not generally recognized by the medical profession…as one of the weapons with which to attack rheumatic conditions.” This attitude persisted until relatively recently, but a systematic review of controlled trials has since shown “a statistically and clinically significant beneficial long-term effect.”
Rheumatoid arthritis has a well-known genetic component, but the concordance rate—that is, the chance that a pair of identical twins both get it when one has it—is probably less than 30 percent, despite the twins having the same genes. That leaves 70 percent to be explained by nongenetic factors.
Even if we don’t know exactly what those factors are, “fasting is very similar to rebooting the hard drive in a computer. Sometimes, the computer gets corrupted and you do not know exactly where the problem is. But if you just turn it off and reboot it, a lot of times, that corruption gets cleared out.”
The evidence base started with case reports of water-only fasting followed by a plant-based diet. There were remarkable reports of years of pain and stiffness that were not only gone within a week but, more importantly, stayed gone on the healthier diet. One after another, just like that. But case reports are merely glorified anecdotes. There have been studies going back decades suggesting that “fasting may represent the most rapid and most available way of inducing relief of arthritic pain and swelling for patients who have RA,” rheumatoid arthritis, but they often failed to control for the placebo effect, which is “particularly important whenever self-reporting systems are used (reports on general well-being, pain, stiffness, tiredness, and the like)”—that is, subjective symptoms. There are objective measures, however, including lab tests of inflammation that don’t appear to be affected by placebos. As shown below and at 3:22 in my video Fasting for Rheumatoid Arthritis is what can be seen in controlled trials, starting immediately and staying down for at least a year.
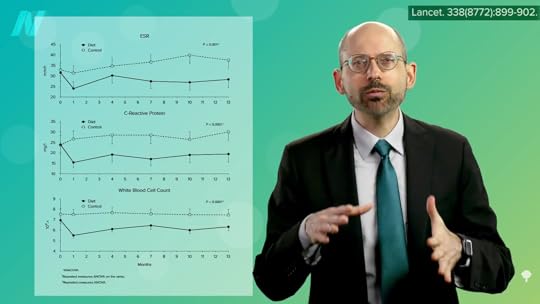
Ten different measures of inflammation decreased significantly after the fasting and subsequent meat- and egg-free diet, whereas none of the parameters budged in those individuals with rheumatoid arthritis who continued to eat their regular diets. What’s more, this squelching of inflammation translated into a significant reduction in pain, morning stiffness, loss of grip strength, and the number of tender and swollen joints, as you can see below and at 3:43 in my video.

Even a year after the trial had ended, those who benefited from the diet continued to benefit in terms of less pain, stiffness, and tender and swollen joints, presumably because they stuck with it, as shown here and at 4:00 in my video.

“There is little doubt that during the period of fasting both inflammation and pain are reduced in RA patients,” individuals with rheumatoid arthritis. “However, after the normal diet is resumed, inflammation returns unless the fasting period is followed by a vegetarian diet…” Why might that be? It could be due to changes in the microbiome. The improvement in symptoms coincided with a “significant alteration in the intestinal flora” when patients switched from an omnivorous diet. “A diet can change intestinal flora and this may somehow be beneficial in RA,” perhaps by strengthening the gut barrier. We know fasting can decrease the leakiness of the gut in individuals with rheumatoid arthritis, but we don’t yet know what role, if any, this plays in the disease process.
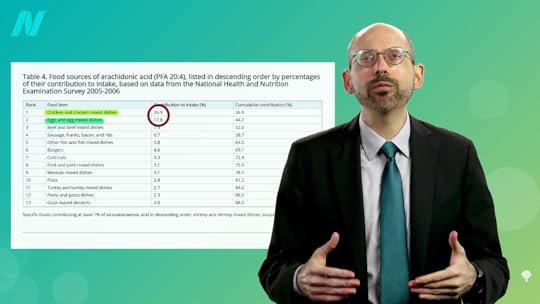
It could be as simple as eicosanoids, the mediators of inflammation that are formed from arachidonic acid. Arachidonic acid is a long-chain, inflammatory, omega-6 fatty acid found in animal fats. As seen below and at 5:04 in my video, the biggest contributors are chicken and eggs, which together contribute nearly half the intake of Americans. That’s also been suggested as an explanation for why those eating more plant-based appear to have better mental health; they aren’t suffering the “cascade of neuroinflammation” caused by arachidonic acid. It’s also why removing eggs, chicken, and other meats was shown to improve mood in a randomized controlled trial, suggesting the arachidonic acid “may negatively impact mood state.” It may also help explain the impact of more plant-based diets on inflammatory diseases like rheumatoid arthritis.
So, all of this may help explain why “maintaining a nutrient-dense, vegan diet of unrefined plant foods”—a plant-based diet—“appears to be necessary after the fast to prevent the recurrence of symptoms and inflammatory activity,” or as one popular press article put it, fasting may just be a tool to get you to radically kickstart a change in the way you eat.
For more on fasting, see related posts below.
This video was originally part of my Fasting for Disease Reversal webinar. If you want to see all of the videos in one place, check them out here.
Stay tuned for Fasting for Autoimmune Diseases, coming up next.
For more on rheumatoid arthritis, see Turmeric Curcumin and Rheumatoid Arthritis, Why Do Plant-Based Diets Help Rheumatoid Arthritis?, and Friday Favorites: Fasting for Rheumatoid Arthritis and Autoimmune Diseases.
December 24, 2024
Cannabis, Strokes, and Heart Attacks?
The temporary quintupling of heart attack risk associated with cannabis smoking may be due to increased heart rate, blood pressure, and carbon monoxide levels.
Does “the dark side of cannabis”—both “synthetic and non-synthetic marijuana”—include stroke?
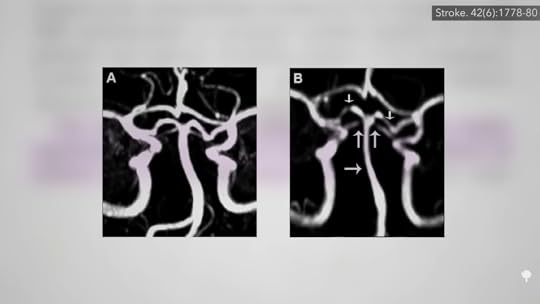
There have been case reports of artery damage due to the “vasoconstrictor effect of cannabis,” which has been well documented. One study found cannabis users had a hundred times greater odds of suffering from multifocal intracranial stenosis, where the arteries inside our brain clamp down at multiple points, as you can see below and at 0:39 in my video Does Marijuana Cause Strokes and Heart Attacks?, but that’s a rare condition. What about strokes?
“The paucity [lack] of high-level evidence regarding the adverse effects of marijuana usage on cerebrovascular [brain artery] health has permitted the false notion that recreational marijuana is safe.” So, researchers decided to put it to the test in a study of millions of cannabis users and found that “recreational marijuana use is independently associated with 17% increased likelihood of AIS hospitalization,” that is, being hospitalized with an acute ischemic stroke, but that may only be among those who use cannabis regularly, “weekly or more often.”
The reason we think it’s cause-and-effect is that the majority of recorded strokes were “during or shortly after marijuana exposure,” and there are even cases in which strokes recurred after re-exposure to marijuana. So, when you put all of that together, it makes a convincing case. Though, to be sure, you’d need to randomize people to use cannabis or a placebo.
It’s like the heart disease story. A similar “temporal” relationship has been found between marijuana use and the development of heart attacks and sudden cardiac death, meaning they seemed to occur while individuals were using cannabis or right after usage. “However, careful evaluation of the cardiovascular effects of marijuana inhalation is complicated by the fact that it is often used in combination with other drugs, such as alcohol or cocaine.” So, you can’t just ask heart attack victims if they were smoking pot at the time of a cardiac event and make the connection; you have to ask about other substance use, too. Within an hour of using cocaine, for example, the risk of having a heart attack goes up more than 20-fold.
That’s about four times more than after smoking pot. The hour after you smoke marijuana, your heart attack risk appears to nearly quintuple, but only for that hour. Then, your risk drops down to normal. So what does this mean? Even though heart disease is our number one killer, the risk of having a heart attack every hour is only about one in a million for any particular hour. So, even if you light up a joint, which may quintuple your risk, that would only bump up the risk to about 1 in 150,000 and only for that one hour. Even if you smoked every day, your annual risk might just go up by a few percentage points. But why the increased risk at all?
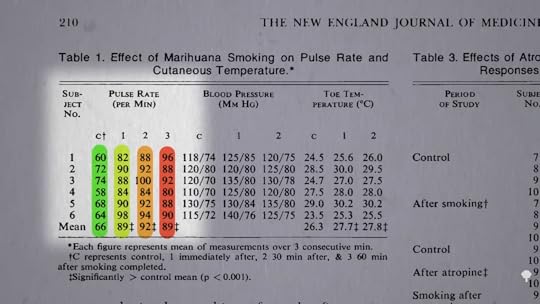
Well, we’ve known since the 1970s that within an hour of smoking a joint, our pulse rate goes up about 35 percent, as you can see below and at 3:20 in my video. Smoking a single joint also increases blood pressure, as well as carbon monoxide levels in the blood of angina patients, and it cuts their ability to exercise nearly in half. Now is that just because they’re breathing in smoke of any kind? No, smoking a placebo joint—that is, a marijuana joint from which the THC has been removed—only cuts down exercise capacity by about 9 percent. In contrast, after smoking an actual cannabis joint, the time the study participants could exercise before experiencing chest pain was cut by 48 percent. So, it does seem to be a specific drug effect. Is it as bad as tobacco? We found that out a year later.
“Smoking 1 marihuana [sic] cigarette decreased the exercise time until angina more than smoking 1 high-nicotine [tobacco] cigarette,” which only cut exercise capacity by 23 percent, compared to 50 percent after the joint. This may be because smoking marijuana seems to put more demand on the heart, so it’s no surprise that it was worse than tobacco.
It may also be carbon monoxide. Smoking marijuana leads to nearly five times more carbon monoxide in the bloodstream than smoking tobacco. This is in part because, compared to cigarette smokers, cannabis smokers inhale more deeply and then hold in the smoke for longer, allowing more carbon monoxide into their system. So, the increased heart rate and pressure, the “cardio acceleration,” may account for the accelerated chest pain in heart disease patients.
Does cannabis have any chronic effects on the arteries? Users do seem to have relatively stiffer arteries for their age, suggesting “an acceleration of the aging process.” We are only as old as our arteries.
Even second-hand marijuana smoke may be harmful, according to a recent study in the Journal of the American Heart Association entitled, “One Minute of Marijuana Secondhand Smoke Impairs Vascular Endothelial Function,” meaning artery function. So, there was a call to protect “vulnerable populations, including elderly and disabled [multi-unit housing] MUH residents, pregnant women, and children.” But, that one minute of exposure to second-hand marijuana smoke was in rats, so it’s not clear how applicable this is to us beyond, perhaps, not smoking around your pets.
I have a slew of other videos on cannabis if you’re interested. Check out the related videos below.
I first released these videos in a webinar, and you can find them all in a digital download here.