Michael Greger's Blog, page 4
May 29, 2025
Celebrating Food, Culture, and AAPI Month with Remy Morimoto Park
We had the pleasure of talking with Remy Morimoto Park about food, culture, and AAPI Month. We hope you enjoy this interview and her recipes for Crunchy Pad Thai Inspired Salad and Miso Soup.

Please tell us a little bit about yourself and your work.
I am a vegan cookbook author and health and wellness content creator. I started Veggiekins blog while I was in college as a means for sharing recipes and spreading the vegan lifestyle, and it has since turned into my full-time job, which has been absolutely incredible. I’m also the founder of a matcha brand, Frauth. Outside of work, I split my time between New York and Los Angeles, and you can usually find me at a farmers market!
In your experience, how have you found food to tell a story and shape culture?
I think that when you come from any type of culture, food is so important because it’s one way culture is passed down from generation to generation. I think that’s why sharing recipes and passing them down is so crucial for preserving culture. In my Asian cultures––Japanese, Korean, and Taiwanese––I think food is really important because it’s also how we communicate with each other and share love. In our cultures, it’s not quite as common to express verbally that you love someone. We really don’t talk too much about feelings, but we always gather around the table to share a meal as a family and many of our holidays and family gatherings revolve around food. There’s a joke that your Asian parents might not apologize or say they love you, but they will always put food on the table for you or cut up a fruit plate for you to communicate that. So, with that in mind, I think that food is a pivotal part of Asian culture. For me personally, a lot of my memories from childhood revolve around a specific meal or have a specific dish tied to it. Food evokes a lot of really powerful memories, and I think it’s a really great vehicle for storytelling in that way.
How do you educate people about the intersection of food, health, community, and culture?
When it comes to most Asian cuisines, there really isn’t very much dairy, which I think is incredible. It also makes them such great foundations for lots of vegan-friendly options. As well, in my three cultures, there are different types of existing plant-based diets followed by religious groups, for example. I think there is a lot to explore, and the same can be said about most cultures. For example, in Korea, there are monks who eat temple food, which is primarily-plant based; in Japan, the Shojin cuisine is also primarily plant-based; and in China, a lot of Buddhists don’t eat any meat or animal products at all. Additionally, my grandparents always told me that, when they were younger, they primarily ate plant-based––mostly grains and vegetables––because meat and animal products were so expensive and reserved more for the higher classes in society. Nowadays, I think people associate meat with Asian cuisine (e.g., Korean BBQ), though, in reality, a lot of Asian cuisine historically revolved around grains and plants.
What are some plant-based ingredients and vegan dishes you would like to highlight as traditional to your cultures and/or other Asian cultures? What are your favorites to cook with?
A plant-based ingredient that I think is essential to Asian culture is tofu, of course! No Asian person is unfamiliar with tofu, and I think that’s incredible because it’s such a great source of plant protein. Rice and other grains are also commonly used throughout Asian cuisines, and some of my personal favourites include tempeh and some of the more unique Asian veggies you wouldn’t typically find at a conventional grocery store (e.g., bean sprouts, bok choy, morning glory, and pea shoots). There’s a great diversity of veggies to choose from in Asian cuisine.
As a plant-based chef, what do you envision as the way forward to encourage people to include more fruits and vegetables into their diets?
One of the things I like to stress the most is that vegetables can be treated with as much care, if not more care, than meat and other animal products. I think a lot of people put in the minimum effort when preparing veggies or may even just eat them raw. When we marinate, smoke, sous vide, roast, or slow cook them, the result is so different.
Nowadays, people have developed this hunger for more global cuisines and are more interested in trying dishes from other cultures, which is a great way to encourage individuals to incorporate more fruits and veggies into their diets. When you start to explore beyond just the United States, for instance, and see what the world has to offer, you find that there are so many different types of fruits and vegetables that you can enjoy. Additionally, there are so many more flavor profiles and spice blends to work with to season your vegetables. Keeping it interesting for the palate is so important!
What significance does AAPI Month have for you, and how do you celebrate your heritage?
AAPI month means a lot to me because I’m not just Asian, but Asian American. I was born in the United States to parents who had already immigrated here and speak primarily English in the house. I don’t feel 100% Asian and, of course, don’t feel 100% American either, so I think that the distinction is really nuanced and makes me feel seen. It’s an incredible sign that people are really embracing others and diversity, which is so important. It’s helped to introduce other cultures to other people and encourage curiosity and hunger for knowledge about others.
I really celebrate my heritage through food and sharing recipes that feel are authentic to my culture and my Asian-American family. It’s such a treat to be able to share that with others and especially to do that plant-based!
Please tell us a little bit about your cookbook, Sesame, Soy, Spice , and what inspired you to write it.
My cookbook was really inspired by my family and my upbringing. “Asian American” is truly the best way to describe my family and the food we eat because we are Asian (and three types of Asian at that), but we are also very much American. Growing up, the food on our table looked like a combination of both western and American foods, as well as the Asian dishes I grew up eating. For example, one thing I love is popcorn, but with Japanese furikake seasoning on top. Sometimes we might sub out chili paste or hot sauce with gochujang, a Korean fermented red pepper paste.
Throughout my cookbook, I really wanted to emphasize that eating vegan does not mean you have to give up your culture and that it can actually be so much fun reconnecting with your culture through trying to recreate those favorite recipes as vegan. It not only makes living a vegan lifestyle more exciting and inclusive, but also more sustainable because there’s more variety in the foods you eat. When I first became vegan, I thought I could only eat foods like salad bowls, grain bowls, and smoothie bowls. Then I realized that it’s not really a diet but a way of life and that almost any cuisine can be vegan-friendly if you get creative in the kitchen.
Through the short stories in my cookbook, I also document my journey to becoming vegan and making peace with my relationship with food. I share the story of how becoming vegan taught me compassion and aided in that journey. The process of writing the cookbook was very meaningful to my family because we really got to connect more than ever through food. I would chat with them about recipes from childhood that I wanted to try to recreate, and we would speak on the phone while we were both in the kitchen, trying to work out a recipe. It was a very nostalgic time for me because, often, we’d end up reminiscing about memories from my childhood while cooking.
Crunchy Pad Thai Inspired Salad
1 to 2 servings, 10 minutes prep
For the Pad Thai Inspired Dressing
½ fresh lime, juiced2 tbsps Umami Sauce 2 tsps tamarind purée1 clove garlic, finely minced1 tbsp rice wine vinegar2 tbsp cashew butter (optional, for creaminess)For the Salad
2 cups shredded purple cabbage3-4 mini cucumbers, julienned1 large carrot, juliennned½ cup chiffonaded radicchio Handful thinly sliced breakfast radishes 1 cup shredded green papaya (optional)Optional
Fresh Thai chili peppersCrushed peanuts to garnishDried chili flakes to garnishGreen onions to garnish
Instructions
In a large bowl, add all the dressing ingredients, then whisk them together. Adjust to taste. If using cashew butter, you may choose to thin it with 1 to 2 tablespoons of water.Add all of the salad ingredients to the bowl, then toss, using your hands or tongs to coat the veggies.Garnish with peanuts, chili flakes, and green onion, if desired.Miso Soup
8 servings, 30 minutes prep, 15 minutes cook time, 30 minutes soaking time
For the Dashi Broth
10 cups filtered water5-6 dried shiitake mushrooms3 kombu pieces (roughly 3 x 3-inches)1 leek stem, sliced diagonally1 carrot, sliced diagonally3 scallions (white parts), halved½ yellow onion, halved12 oz firm silken tofu¼ cup dried wakameOther Ingredients
5 tbsps red miso paste5 tbsps white miso pasteFor Garnish
Scallions (green tops), thinly slicedIchimi togarashi, to tasteCooked mushrooms (optional)
Instructions
Prepare Dashi Broth
To your cooking pot, add the water, dried mushrooms, and kombu. Let soak for about 15 to 30 minutes. (The longer you soak, the more flavor will be released).Bring to a boil, then lower the heat to a simmer. Let simmer for 10 minutes.Add the leek, carrots, scallions, and onion, and cook for another 10 minutes.Add the tofu, then remove the pot from the heat.Re-Hydrate Wakame
In a small bowl, add the dried wakame with enough hot water to cover. Let soak until the wakame is soft to the touch, then drain and set aside.Add Miso Paste
In a small jar or bowl, add the red and white miso with a little water. You want to add just enough water so the misos turn into a thin paste. Use a whisk or chopsticks to break down the paste so it’s pourable. Add the wakame and the whisked miso to the pot, and gently stir to combine. Adjust to taste.Garnish with green scallion tops, ichimi togarashi, and cooked mushrooms, if desired.For more about Remy, check out her blog, Instagram, TikTok, and YouTube.
May 27, 2025
Food Safety and Cultivated Meat
What are the direct health implications of making clean meat—that is, meat without animals?
In a 1932 article in Popular Mechanics entitled “Fifty Years Hence,” Winston Churchill predicted that we would one day “escape the absurdity of growing a whole chicken in order to eat the breast or wing, by growing these parts separately under a suitable medium.” Indeed, growing meat straight from muscle cells could reduce greenhouse gas emissions by as much as 96 percent, lower water usage by as much as 96 percent, and lower land usage by 99 percent.
If we are to avoid dangerous climate change by the middle of the century, global meat consumption simply cannot continue to rise at the current rate. And there have certainly been initiatives like Meatless Mondays to try to get people to cut down, but so far, “they do not appear to be contributing in any significant way to the translation of the idea of eating less meat into the mainstream.” So, “in the light of people’s continued desire to eat meat, it seems the problems associated with consumption are unlikely to be fully resolved by attitude change. Instead, they must be addressed from an alternate perspective: changing the product.”
From an environmental standpoint, it seems like a slam dunk. From an animal welfare standpoint, it could get rid of factory farms and slaughter plants for good, and I wouldn’t have to stumble across articles like this in the scientific literature: “Discerning Pig Screams in Production Environments.” I mean, what more do we need to know about modern animal agriculture than the fact that, “in recent years, a number of so-called…‘ag-gag’ laws have been proposed and passed…across the USA,” banning undercover photographing or videotaping inside such operations to keep us all in the dark.
What about the human health implications of cultivated meat? I get the animal welfare, environment, and food security benefits, but what about “the potential for cultured meat to have health/safety benefits to individual consumers”? Nutritionally, the most important advantage is being able to swap out the type the fat. Right now, producers are growing straight muscle tissue, so it could be marbled with something less harmful than animal fat, though, of course, there’s still animal protein.
When it comes to health, the biggest, clearest advantage is food safety, reducing the risk of foodborne pathogens. There has been a sixfold increase in food poisoning over the last few decades, with tens of millions “sickened annually by infected food in the United States alone,” including hundreds of thousands of hospitalizations and thousands of annual deaths. Contaminated meats and other animal products are the most common cause.
When the cultivated meat industry calls its products clean meat, that’s not just a nod to clean energy. Food-poisoning pathogens like E. coli, Campylobacter, and Salmonella are fecal bacteria. They are a result of fecal contamination. They’re intestinal bugs, so we don’t have to worry about them if we’re making meat without the intestines.
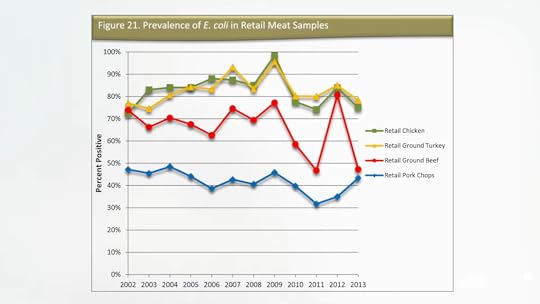
Yes, there are all sorts of “methods to remove visible fecal contamination” in slaughter plants these days and even experimental imaging technologies designed to detect more “diluted fecal contaminations,” but we are still left at the retail level with about 10 percent of chicken contaminated with Salmonella and 40 percent of retail chicken contaminated with Campylobacter. What’s more, most poultry and about half of retail ground beef and pork chops are contaminated with E. coli, an indicator of fecal residue, as shown here and at 3:47 in my video The Human Health Effects of Cultivated Meat: Food Safety. We don’t have to cook the crap out of cultivated meat, though, because there isn’t any crap to begin with.
Doctor’s Note:
This is the first in a three-video series on cultivated meat. Stay tuned for The Human Health Effects of Cultivated Meat: Antibiotic Resistance and The Human Health Effects of Cultivated Meat: Chemical Safety.
I previously did a video series on plant-based meats. Check them in the related posts below.
The videos are also all available in a digital download from a webinar I did: The Human Health Implications of Plant-Based and Cultivated Meat for Pandemic Prevention and Climate Mitigation.
May 22, 2025
Statins and Muscle Pain Side Effects
Why is the incidence of side effects from statins so low in clinical trials while appearing to be so high in the real world?
“There is now overwhelming evidence to support reducing LDL-C (low-density lipoprotein cholesterol)”—so-called bad cholesterol—to reduce atherosclerotic cardiovascular disease (CVD),” the number one killer of men and women. So, why is adherence to cholesterol-lowering statin drug therapy such “a major challenge worldwide”? Researchers found “that the majority of studies reported that at least 40%, and as much as 80%, of patients did not comply fully with statin treatment recommendations.” Three-quarters of patients may flat out stop taking them, and almost 90 percent may discontinue treatment altogether.
When asked why they stopped taking the pills, most “former statin users or discontinuers…cited muscle pain, a side effect, as the primary reason…” “SAMSs”—statin-associated muscle symptoms—“are by far the most prevalent and important adverse event, with up to 72% of all statin adverse events being muscle-related.” Taking coenzyme Q10 supplements as a treatment for statin-associated muscle symptoms was a good idea in theory, but they don’t appear to help. Normally, side-effect symptoms go away when you stop the drug but can sometimes linger for a year or more. There is “growing evidence that statin intolerance is predominantly psychosocial, not pharmacological.” Really? It may be mostly just in people’s heads?
“Statins have developed a bad reputation with the public, a phenomenon driven largely by proliferation on the Internet of bizarre and unscientific but seemingly persuasive criticism of these drugs.” “Does Googling lead to statin intolerance?” But people have stopped taking statins for decades before there even was an Internet. What kinds of data have doctors suggested that patients are falsely “misattribut[ing] normal aches and pains to be statin side effects”?
Well, if you take people who claim to have statin-related muscle pain and randomize them back and forth between statins and an identical-looking placebo in three-week blocks, they can’t tell whether they’re getting the real drug or the sugar pill. The problem with that study, though, is that it may take months not only to develop statin-induced muscle pain, but months before it goes away, so no wonder three weeks on and three weeks off may not be long enough for the participants to discern which is which.
However, these data are more convincing: Ten thousand people were randomized to a statin or a sugar pill for a few years, but so many more people were dying in the sugar pill group that the study had to be stopped prematurely. So then everyone was offered the statin, and the researchers noted that there was “no excess of reports of muscle-related AEs” (adverse effects) among patients assigned to the statin over those assigned to the placebo. But when the placebo phase was over and the people knew they were on a statin, they went on to report more muscle side effects than those who knew they weren’t taking the statin. “These analyses illustrate the so-called nocebo effect,” which is akin to the opposite of the placebo effect.
Placebo effects are positive consequences falsely attributed to a treatment, whereas nocebo effects are negative consequences falsely attributed to a treatment, as was evidently seen here. There was an excess rate of muscle-related adverse effects reported only when patients and their doctors were aware that statin therapy was being used, and not when its use was concealed. The researchers hope “these results will help assure both physicians and patients that most AEs associated with statins are not causally related to use of the drug and should help counter…exaggerated claims about statin-related side effects.”
These are the kinds of results from “placebo-controlled randomised trials [that] have shown definitively that almost all of the symptomatic adverse events that are attributed to statin therapy in routine practice are not actually caused by it (ie, they represent misattribution.)” Now, “only a few patients will believe that their SAMS are of psychogenic origin” and just in their head, but their denial may have “deadly consequences.” Indeed, “discontinuing statin treatment may be a life-threatening mistake.”
Below and at 4:46 in my video How Common Are Muscle Side Effects from Statins?, you can see the mortality of those who stopped their statins after having a possible adverse reaction compared to those who stuck with them. This translates into about “1 excess death for every 83 patients who discontinued treatment” within a four-year period. So, when there are media reports about statin side effects and people stop taking them, this could “result in thousands of fatal and disabling heart attacks and strokes, which would otherwise have been avoided. Seldom in the history of modern therapeutics have the substantial proven benefits of a treatment been compromised to such an extent by serious misrepresentations of the evidence for its safety.” But is it a misrepresentation to suggest “that statin therapy causes side-effects in up to one fifth of patients”? That is what is seen in clinical practice; between 10 to 25 percent of patients placed on statins complain of muscle problems. However, because we don’t see anywhere near those kinds of numbers in controlled trials, patients are accused of being confused. Why is the incidence of side effects from statins so low in clinical trials while appearing to be so high in the real world?

Take this meta-analysis of clinical trials, for example: It found muscle problems not in 1 in 5 patients, but only 1 in 2,000. Should everyone over a certain age be on statins? Not surprisingly, every one of those trials was funded by statin manufacturers themselves. So, for example, “how could the statin RCTs [randomized controlled trials] miss detecting mild statin-related muscle adverse side effects such as myalgia [muscle pain]? By not asking. A review of 44 statin RCTs reveals that only 1 directly asked about muscle-related adverse effects.” So, are the vast majority of side effects just being missed in all these trials, or are the vast majority of side effects seen in clinical practice just a figment of patients’ imagination? The bottom line is we don’t know, but there is certainly an urgent need to figure it out.
May 20, 2025
Eating to Treat Crohn’s Disease
Switching to a plant-based diet has been shown to achieve far better outcomes than those reported on conventional treatments for both active and quiescent stages of Crohn’s disease (CD) and ulcerative colitis.
Important to our understanding and the prevention of the global increase of inflammatory bowel disease (IBD), we know that “dietary fiber reduces risk, whereas dietary fat, animal protein, and sugar increase it.” “Despite the recognition of westernization of lifestyle as a major driver of the growing incidence of IBD, no countermeasures against such lifestyle changes have been recommended, except that patients with Crohn’s disease should not smoke.”
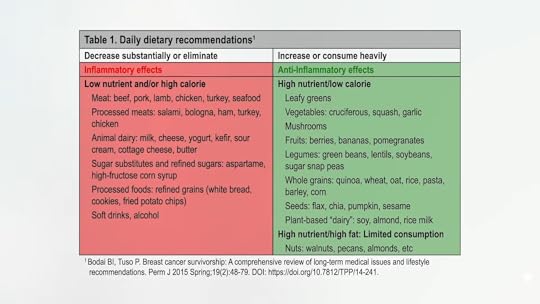
We know that “consuming whole, plant-based foods is synonymous with an anti-inflammatory diet.” Lists of foods with inflammatory effects and anti-inflammatory effects are shown here and at 0:50 in my video, The Best Diet for Crohn’s Disease.
How about putting a plant-based diet to the test?
Cutting down on red and processed meats didn’t work, but what about cutting down on all meat? A 25-year-old man “with newly diagnosed CD…failed to enter clinical remission despite standard medical therapy. After switching to a diet based exclusively on grains, legumes [beans, split peas, chickpeas, and lentils], vegetables, and fruits, he entered clinical remission without need for medication and showed no signs of CD on follow-up colonoscopy.”
It’s worth delving into some of the details. The conventional treatment he was started on is infliximab, sold as REMICADE®, which can cause a stroke and may increase our chances of getting lymphoma or other cancers. (It also costs $35,000 a year.) It may not even work in 35 to 40 percent of patients, and that seemed to be the case with the 25-year-old man. So, his dose was increased after 37 weeks, but he was still suffering after two years on the drug. Then he completely eliminated animal products and processed foods from his diet and finally experienced a complete resolution of his symptoms.
“Prior to this, his diet had been the typical American diet, consisting of meat, dairy products, refined grains, processed foods, and modest amounts of vegetables and fruits. Having experienced complete clinical remission for the first time since his Crohn’s disease diagnosis, the patient decided to switch to a whole food, plant-based diet permanently, severely reducing his intake of processed foods and limiting animal products to one serving, or less, per week.” Whenever his diet slipped, his symptoms started coming back, but he could always eliminate them by eating healthier again. After six months adhering to these diet and lifestyle changes, including stress relief and exercise, a follow-up “demonstrated complete mucosal healing [of the gut lining] with no visible evidence of Crohn’s disease.”
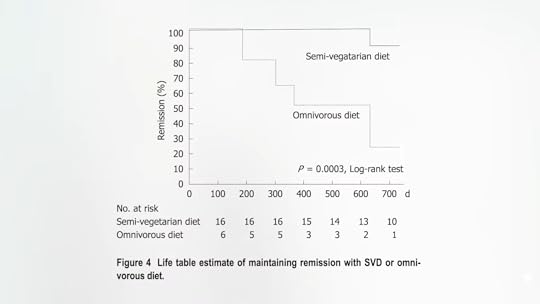
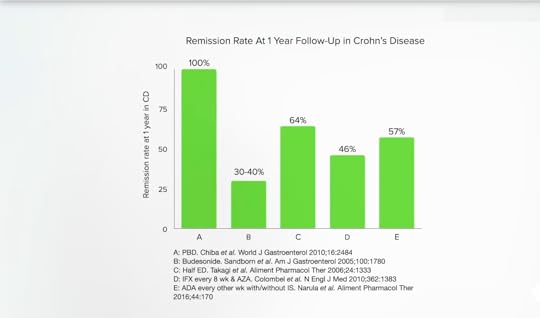
We know that “a diet consisting of whole grains, legumes, fruits, and vegetables has been shown to be helpful in the prevention and treatment of heart disease, obesity, diabetes, hypertension, gallbladder disease, rheumatoid arthritis, and many cancers. Although further research is required, this case report suggests that Crohn’s disease might be added to this list of conditions.” That further research has already been done! About 20 patients with Crohn’s disease were placed on a semi-vegetarian diet—no more than half a serving of fish once a week and half a serving of meat once every two weeks—and they achieved a 100 percent remission rate at one year and 90 percent at two years.
Some strayed from the diet, though. What happened to them? As you can see below and at 3:32 in my video, after one year, half had relapsed, and, at year two, only 20 percent had remained in remission. But those who stuck with the semi-veg diet had remarkable success. It was a small study with no formal control group, but it represents the best-reported result in Crohn’s relapse prevention published in the medical literature to date.
Nowadays, Crohn’s patients are often treated with so-called biologic drugs, expensive injected antibodies that suppress the immune system. They have effectively induced and maintained remission in Crohn’s disease, but not in everybody. The current remission rate in Crohn’s with early use of REMICADE® is 64 percent. So, 30 to 40 percent of patients “are likely to experience a disabling disease course even after their first treatment.” What about adding a plant-based diet? Remission rates jumped up to 100 percent for those who didn’t have to drop out due to drug side effects. Even after excluding milder cases, researchers found that 100 percent of those with serious, even “severe/fulminant disease, achieved remission.”
If we look at gold standard systematic reviews, they conclude that the effects of dietary interventions on inflammatory bowel diseases—Crohn’s disease and ulcerative colitis—are uncertain. However, this is because only randomized controlled trials were considered. That’s totally understandable, as that is the most rigorous study design. “Nevertheless, people with IBD deserve advice based on the ‘best available evidence’ rather than no advice at all…” And switching to a plant-based diet has been shown to achieve “far better outcomes” than those reported on conventional treatments in both active and quiescent stages in Crohn’s disease and ulcerative colitis. For example, below and at 5:37 in my video, you can see one-year remission rates in Crohn’s disease (100 percent) compared to budesonide, an immunosuppressant corticosteroid drug (30 to 40 percent), a half elemental diet, such as at-home tube feedings (64 percent), the $35,000-a-year drug REMICADE® (46 percent), or the $75,000-a-year drug Humira (57 percent).
Safer, cheaper, and more effective. That’s why some researchers have made the “recommendation of plant-based diets for inflammatory bowel disease.”
It would seem clear that treatment based on addressing the cause of the disease is optimal. Spreading the word about healthier diets could help halt the scourge of inflammatory bowel disease, but how will people hear about this amazing research without some kind of public education campaign? That’s what NutritionFacts.org is all about.
Doctor’s Note:
This is the third in a series on inflammatory bowel disease. If you missed the first two, see Preventing Inflammatory Bowel Disease with Diet and The Best Diet for Ulcerative Colitis Treatment.
My previous Crohn’s videos include Preventing Crohn’s Disease with Diet and Does Nutritional Yeast Trigger Crohn’s Disease?.
May 15, 2025
Eating to Keep Ulcerative Colitis in Remission
Plant-based diets can be 98 percent effective in keeping ulcerative colitis patients in remission, far exceeding the efficacy of other treatments.
“One of the most common questions physicians treating patients with IBD [inflammatory bowel disease] are asked is whether changing diet could positively affect the course of their disease.” Traditionally, we had to respond that we didn’t know. That may now be changing, given the “evidence in the literature that hydrogen sulfide may play a role in UC,” ulcerative colitis. And, since the sulfur-containing amino acids concentrated in meat cause an increase in colonic levels of this rotten egg gas, perhaps we should “take off the meat.” Indeed, animal protein isn’t associated only with an increased risk of getting inflammatory bowel disease in the first place, but also IBD relapses once you have the disease.
This is a recent development. “Because the concept of IBD as a lifestyle disease mediated mainly by a westernized diet is not widely appreciated, an analysis of diet in the follow-up period [after diagnosis] in relation to a relapse of IBD has been ignored”—but no longer. Ulcerative colitis patients in remission and their diets were followed for a year to see which foods were linked to the return of their bloody diarrhea. Researchers found that the “strongest relationship between a dietary factor and an increased risk of relapse observed in this study was for a high intake of meat,” as I discuss in my video The Best Diet for Ulcerative Colitis Treatment.
What if people lower their intake of sulfur-containing amino acids by decreasing their consumption of animal products? Researchers tried this on four ulcerative colitis patients, and without any change in their medications, the patients experienced about a fourfold improvement in their loose stools. In fact, they felt so much better that the researchers didn’t think it was ethical to try switching the patients back to their typical diets. “Sulfur-containing amino acids are the primary source of dietary sulfur,” so a “low-sulfur” diet essentially means “a shift from a more traditional western diet (high in animal protein and fat, and low in fiber) to more of a plant-based diet (high in fiber, lower in animal protein and fat).” “Altogether, westernized diets are pro-inflammatory, and PBD [plant-based diets] are anti-inflammatory.”
What can treatment with a plant-based diet do after the onset of ulcerative colitis during a low-carbohydrate weight-loss diet? A 36-year-old man lost 13 pounds on a low-carb diet, but he also lost his health; he was diagnosed with ulcerative colitis. When he was put on a diet centered around whole plant foods, his symptoms resolved without medication. He achieved remission. That was just one case, though. Case reports are akin to glorified anecdotes. The value of case reports lies in their ability to inspire researchers to put them to the test, and that’s exactly what they did.
Until then, there had never been a study published that focused on using plant-based diets for treating ulcerative colitis. Wrote the researchers, a group of Japanese gastroenterologists, “We consider that the lack of a suitable diet is the biggest issue faced in the current treatment of IBD. We regard IBD as a lifestyle disease caused mainly by our omnivorous (Western) diet. We have been providing a plant-based diet (PBD) to all patients with IBD” for more than a decade and have published extraordinary results, far better than have been reported elsewhere in the medical literature to date. (I profiled some of their early work in one of the first videos that went up on NutritionFacts.org.) The researchers found a plant-based diet to be “effective in the maintenance of remission” in Crohn’s disease by 100 percent at one year and 90 percent at two years. What about a plant-based diet for relapse prevention in ulcerative colitis?
“Educational hospitalization” involved bringing patients into the hospital to control their diet and educate them about the benefits of plant-based eating (so they’d be more motivated to continue it at home). “Most patients (77%) experienced some improvement, such as disappearance or decrease of bloody stool during hospitalization.” Fantastic!
Here’s the really exciting part. The researchers then followed the patients for five years, and 81 percent of them remained in remission for the entire five years, and 98 percent kept the disease at bay for at least one year. That blows away other treatments. Those relapse rates are far lower than those reported with medication. Under conventional treatment, other studies found that about half of the individuals relapse, compared to only 2 percent of those taught to eat healthier.
“A PBD was previously shown to be effective in both the active and quiescent stages of Crohn’s disease. The current study showed that a PBD is effective in both the active and quiescent stages of UC as well.” So, the researchers did another study on even more severely affected cases with active disease and found the same results, with plant-based eating beating conventional drug therapy by far. People felt so much better that they were still eating more plant-based food even six years later. The researchers conclude that a plant-based diet is effective for treating ulcerative colitis to prevent a relapse.
Why? Well, plant-based diets are rich in fiber, which feeds our good gut bugs. “This observation might partly explain why a PBD prevents a variety of chronic diseases. Indeed, the same explanation applies to IBD, indicating that replacing an omnivorous diet with a PBD in IBD is the right approach.”
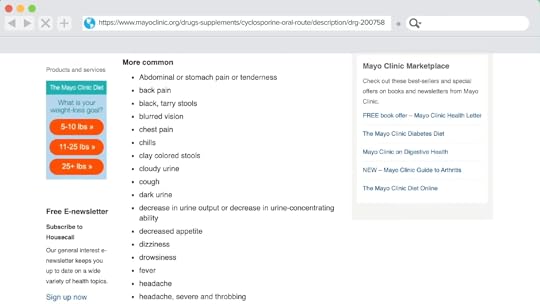
It’s like using plant-based diets to treat the cause of heart disease, our number one killer. Plant-based eating isn’t only safer and cheaper, but it also works better with no noted adverse side effects. Let’s compare that to the laundry list of side effects of immunosuppressants used for ulcerative colitis, like cyclosporine, which you can see below and at 5:40 in my video.
We now have even fancier drugs costing about $60,000 a year, about $5,000 a month, and they don’t even work very well; clinical remission at one year is only about 17 to 34 percent. And, instead of no adverse side effects, the drugs can give us a stroke, give us heart failure, and can even give us cancer, including a rare type of cancer that often results in death. Also, a serious brain disease known as progressive multifocal leukoencephalopathy, which can kill us, and for which there is no known treatment or cure. One drug lists an “increased risk of death” but touts that it’s just “a small pill” in an “easy-to-open bottle.” I’d skip the pills (and their potential side effects) and stick with plant-based eating.
Doctor’s Note:
If you missed the previous video, see Preventing Inflammatory Bowel Disease with Diet and stay tuned for The Best Diet for Crohn’s Disease Treatment, coming up next.
Check the related posts below for some older videos on IBD that may be of interest to you.
May 13, 2025
Foods That Disrupt Our Microbiome
Eating a diet filled with animal products can disrupt our microbiome faster than taking an antibiotic.
If you search online for “Crohn’s disease and diet” or “ulcerative colitis and diet,” the top results are a hodgepodge of conflicting advice, as you can see below and at 0:15 in my video Preventing Inflammatory Bowel Disease with Diet.

What does science say? A systematic review of the medical literature on dietary intake and the risk of developing inflammatory bowel disease finds that Crohn’s disease is associated with the intake of fat and meat, whereas dietary fiber and fruits appear protective. The same associations are seen with ulcerative colitis, the other major inflammatory bowel disease—namely, increased risk with fat and meat, and a protective association with vegetable intake.
Why, according to this meta-analysis of nine separate studies, do meat consumers have about a 50 percent greater risk for inflammatory bowel disease? One possibility is that meat may be a vehicle for bacteria that play a role in the development of such diseases. For instance, meat contains “huge amounts of Yersinia.” It’s possible that antibiotic residues in the meat itself could be theoretically mucking with our microbiome, but Yersinia are so-called psychotropic bacteria, meaning they’re able to grow at refrigerator temperatures, and they’ve been found to be significantly associated with inflammatory bowel disease (IBD). This supports the concept that Yersinia infection may be a trigger of chronic IBD.
Animal protein is associated with triple the risk of inflammatory bowel disease, but plant protein is not, as you can see below and at 1:39 in my video. Why? One reason is that animal protein can lead to the formation of toxic bacterial end products, such as hydrogen sulfide, the rotten egg gas. Hydrogen sulfide is not just “one of the main malodorous compounds in human flatus”; it is a “poison that has been implicated in ulcerative colitis.” So, if you go on a meat-heavy, low-carb diet, we aren’t talking just about some “malodorous rectal flatus,” but increased risk of irritable bowel syndrome, inflammatory bowel syndrome (ulcerative colitis), and eventually, colorectal cancer.
Hydrogen sulfide in the colon comes from sulfur-containing amino acids, like methionine, that are concentrated in animal proteins. There are also sulfites added as preservatives to some nonorganic wine and nonorganic dried fruit, but the sulfur-containing amino acids may be the more important of the two. When researchers gave people increasing quantities of meat, there was an exponential rise in fecal sulfides, as seen here and at 2:37 in my video.

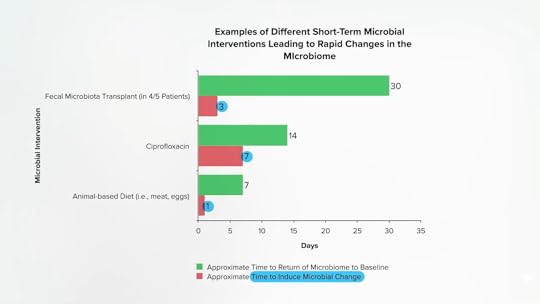
Specific bacteria, like Biophilia wadsworthia, can take this sulfur that ends up in our colon and produce hydrogen sulfide. Eating a diet based on animal products, packed with meat, eggs, and dairy, can specifically increase the growth of this bacteria. People underestimate the dramatic effect diet can have on our gut bacteria. As shown below and at 3:12 in my video, when people are given a fecal transplant, it can take three days for their microbiome to shift. Take a powerful antibiotic like Cipro, and it can take a week. But if we start eating a diet heavy in meat and eggs, within a single day, our microbiome can change—and not for the better. The bad bacterial machinery that churns out hydrogen sulfide can more than double, and this is consistent with the thinking that “diet-induced changes to the gut microbiota [flora] may contribute to the development of inflammatory bowel disease.” In other words, the increase in sulfur compounds in the colon when we eat meat “is not only of interest in the field of flatology”—the study of human farts—“but may also be of importance in the pathogenesis of ulcerative colitis…”
Doctor’s Note:
This is the first in a three-part video series. Stay tuned for The Best Diet for Ulcerative Colitis Treatment and The Best Diet for Crohn’s Disease Treatment.
May 8, 2025
Skincare as You Age Infographic
When I dove into the scientific research for my book How Not to Age, I uncovered the best ways we can care for our skin as we mature. What are the most important lifestyle factors? The best topical creams? Are there any beneficial procedures? This infographic summarizes the main takeaways.


Get this infographic as a downloadable PDF with citations here.
For more details about the studies referenced in this infographic, watch the related videos for free on NutritionFacts.org’s YouTube channel or on our website’s Anti-aging topic page.
May 6, 2025
Treating Fatty Liver Disease with Diet
What are the three sources of liver fat in fatty liver disease, and how can we get rid of it?
Nonalcoholic fatty liver disease (NAFLD) is now the most frequent chronic liver disease, thanks in part to our epidemic of obesity, and is even seen in children. “[N]early 70–80% of obese children may have NAFLD.” Why do we care? Because a fatty liver can progress into fatty hepatitis, which can cause scarring and liver cirrhosis, and cirrhosis is bad enough, but it may also cause the development of liver cancer.
What is the source of the liver fat in fatty liver disease? There are three main sources: the excess sugar in our diet, the excess fat in our diet, and the fat spilling over from our excess body fat, as you can see at 0:51 in my video The Best Diet for Fatty Liver Disease Treatment.

How do we know excess dietary sugar is bad? Because it’s been put to the test. When teens with fatty liver disease were randomized to a diet low in free sugars (meaning a diet low in added sugar and sugary beverages), they experienced a significant improvement within eight weeks. Given these new data, a liver journal editorial read that “a strong argument can be made that we are beyond any period of uncertainty about the harmful effects of excess sugar consumption and that we must now act on the large body of available data to inform the public of the health risks of eating too much sugar.”
And how do we know excess dietary fat is bad? Because it’s also been put to the test. When people were randomized to a low-fat diet or a high-fat diet with the same number of calories, within just two weeks, the liver fat of those on the low-fat diet decreased by 20 percent, whereas it increased by 35 percent in the participants getting the same number of calories but on a high-fat diet.
On the low-fat diet, insulin levels went down about 15 percent, and on the high-fat diet, insulin levels went up about 15 percent. Low-carbohydrate and ketogenic diet advocates often talk about how we need to eat more fat and less carbs to keep our insulin levels down, but the exact opposite happens when it’s actually put to the test. A single high-fat meal not only increases liver fat but also insulin resistance. Within four hours, our whole-body insulin sensitivity can drop by 25 percent, so our body has to pump out that much more insulin. As the accompanying editorial put it: “A single fat bolus [dose] packs a punch.”
So, to help prevent or treat fatty liver disease, patients should limit or avoid eating foods rich in fats. While more long-term clinical trials are always needed, “based on current evidence, we would recommend a diet low in fat, notably in saturated fatty acids, and low in refined carbohydrates, notably by reducing soft drinks consumption…as these nutritional factors may play a pivotal role in NAFLD.” So that means a diet low in meat, dairy, junk, and refined carbs, especially soda. Saturated fat is not only “more metabolically harmful for the human liver than unsaturated fat,” but saturated fat is more harmful than straight sugar. What happened when study participants were overfed with 1,000 calories of saturated fat (like cheese and coconut oil), unsaturated fat (like nuts and olive oil), or sugar (like soda and candy)? Overeating 1,000 calories a day of anything isn’t good for us, but the saturated fat increased liver fat by 55 percent, significantly more than the unsaturated fats, with the candy coming in between the two.
So, “although weight loss is beneficial in NAFLD, certain diets known to induce weight loss can actually cause or exacerbate this disease, and therefore induce insulin resistance, such as very low carbohydrate, high fat diets.” In contrast, “healthy plant-based diets are associated with lower NAFLD risk and more favorable liver function tests profile.” The consumption of legumes (beans, split peas, chickpeas, and lentils), for example, is associated with a lower risk of fatty liver, up to 65 percent lower odds from eating more beans.
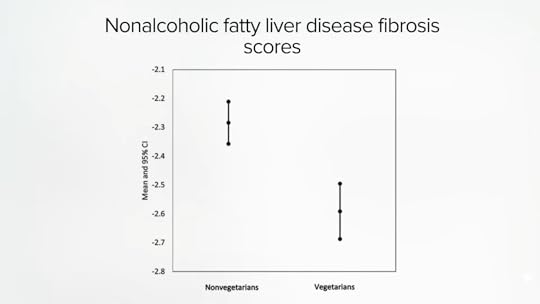
In the earlier study, researchers weren’t looking at people eating strictly plant-based diets, just more or less so. It’s harder to study those eating completely meat-free diets since they currently represent just a small segment of the U.S. population. But what about Americans of Indian descent? South Asians, individuals originating from the Indian subcontinent, are “one of the fastest growing ethnic groups in the United States,” and they appear to largely retain their diets, with about the same percentage of vegetarians as in India—nearly 40 percent. We know that in India, meat eaters are at significantly higher risk of fatty liver disease. It is the same in Taiwan, with vegetarians at significantly lower risk of fatty liver. And even the vegetarians who were affected had significantly less liver scarring, as you can see below and at 4:35 in my video. Their data suggest that “replacing a serving of soy with a serving of meat or fish was associated with 12%-13 % increased risk”—having a single serving of meat instead of soy elevates the risk of fatty liver.
And in the United States? Eating a vegetarian diet was associated with being slimmer and having better blood sugars, better cholesterol, and less than half the odds of fatty liver disease. Is it cause and effect? We have to put it to the test. In an effort to reverse a fatty liver patient’s inflammatory bowel disease with a plant-based diet, researchers found that their liver inflammation was dramatically improved, but they also lost about nine pounds in the first 11 days, thanks to eating healthfully, so it’s hard to tease out the specific effects of the diet on its own. In fact, we have to be careful about rapid weight loss, because all that extra fat being broken down can flood into the bloodstream and sometimes make things worse. So, for individuals with fatty liver disease, losing about three pounds a week might be safer.
Even though a plant-based diet has yet to be properly put to the test in a randomized clinical trial for fatty liver disease, I would submit that it is still the best diet for this disease, and that isn’t based on a single case report, but on the fact that cardiovascular disease, not liver failure, is the most common cause of death among patients with fatty liver disease. And we do have randomized controlled trials proving that a healthy plant-based diet and lifestyle programs can reverse heart disease and open up arteries without drugs, surgery, or stents. Yes, patients with fatty liver disease and fatty hepatitis “may eventually develop cirrhosis [of the liver], but only if they do not die of cardiovascular diseases first.”
Doctor’s Note:
There are some specific foods that may also help. See my videos in the related posts below.
If excess sugar is so bad, what about fruit? Check out If Fructose Is Bad, What About Fruit? and How Much Fruit Is Too Much?.
May 2, 2025
Bird Flu: Emergence, Dangers, and Preventive Measures
In the United States in January 2025 alone, approximately 20 million commercially-raised birds, mostly egg-laying hens, were affected by the highly pathogenic avian influenza (H5N1). These numbers are staggering yet barely scratch the surface of a potentially larger threat looming over the country. If action is not taken now, the next pandemic could be far deadlier than the 1918 influenza and COVID-19.
What Was the 1918 Influenza?
According to the World Health Organization (WHO), “The 1918 influenza pandemic killed more people in less time than any other disease before or since”; it was the “most deadly disease event in the history of humanity.” Indeed, it killed more people in a single year than the bubonic plague—the “black death”—in the Middle Ages killed in a century. The 1918 virus also killed more people in twenty-five weeks than AIDS killed in twenty-five years. According to one academic reviewer, this “single, brief epidemic generated more fatalities, more suffering, and more demographic change in the United States than all the wars of the Twentieth Century.”
What Caused the 1918 Flu Pandemic?
Although the human influenza virus wasn’t even discovered until 1933, an inspector with the U.S. Bureau of Animal Industry had been publishing research as early as 1919 that suggested a role for farm animals in the pandemic. Inspector J.S. Koen of Fort Dodge, Iowa, wrote: “The similarity of the epidemic among people and the epidemic among pigs was so close, the reports so frequent, that an outbreak in the family would be followed immediately by an outbreak among the hogs, and vice versa, as to present a most striking coincidence if not suggesting a close relation between the two conditions. It looked like ‘flu,’ and until proven it was not ‘flu,’ I shall stand by that diagnosis.”
The answer to where the 1918 virus came from was published in October 2005. Humanity’s greatest killer appeared to originally come from avian influenza—bird flu.
What Is Bird Flu?
Evidence now suggests that all pandemic influenza viruses—in fact all human and mammalian flu viruses in general—owe their origins to avian influenza. Back in 1918, schoolchildren jumped rope to a morbid little rhyme:
I had a little bird,
Its name was Enza.
I opened the window,
And in-flu-enza.
Is Bird Flu Worse Than Regular Flu?
As devastating as the 1918 pandemic was, the mortality rate was less than 5 percent on average. But the H5N1 strain of bird flu virus that first emerged in China in 1997 and spread to more than 60 countries seems to kill about 50 percent of its known human victims, on par with some strains of Ebola, making it potentially ten times as deadly as the worst plague in human history.
Leading public health authorities, from the U.S. Centers for Disease Control and Prevention (CDC) to the World Health Organization, feared that this bird flu virus was but mutations away from spreading efficiently though the human population, triggering the next pandemic. “The lethal capacity of this virus is very, very high; so it’s a deadly virus that humans have not been exposed to before. That’s a very bad combination,” said Irwin Redlener, former director of the National Center for Disaster Preparedness at Columbia University. Scientists speculate worst-case scenarios in which H5N1 could end up killing a billion or more people around the world. “The only thing I can think of that could take a larger human death toll would be thermonuclear war,” said Council on Foreign Relations senior fellow Laurie Garrett. H5N1 has the potential to become a virus as ferocious as Ebola and as contagious as the common cold.
H1N1 vs. H5N1
The 1918 pandemic virus was H1N1. The annual flu strain remained H1N1, infecting relatively few people every year for decades until 1957, when an H2N2 virus suddenly appeared as the “Asian flu” pandemic. Because the world’s population had essentially only acquired immunity to H1 spikes, the virus raced around the globe, infecting a significant portion of the world’s population. For example, half of U.S. schoolchildren fell ill. H2N2 held seasonal sway for 11 years. In 1968, the H3N2 “Hong Kong Flu” virus triggered another pandemic and has been with us every year since.
So there were three influenza pandemics in the twentieth century—in 1918, 1957, and 1968—but, as the director of the National Institute for Allergy and Infectious Diseases has said, “There are pandemics and then there are pandemics.” The half-and-half bird/human hybrid viruses of 1957 and 1968 evidently contained enough previously recognizable human structure that the human population’s prior partial exposure dampened the pandemic’s potential to do harm. In contrast, the pandemic strain of 1918 was wholly avian-like. Instead of diluting its alien avian nature, the 1918 bird flu virus “likely jumped straight to humans and began killing them,” noted Taubenberger, the man who helped resurrect it. The same could be happening with the new spate of avian influenza viruses sporadically infecting people in more recent years, like H5N1. The human immune system had never been known to be exposed to an H5 virus before. As the WHO points out, “Population vulnerability to an H5N1-like pandemic virus would be universal.”
How Dangerous Is H5N1 Bird Flu?
H5N1 developed a level of human lethality not thought possible for influenza. So far, about half of those known to have come down with this flu have died. H5N1 is good at killing, but not at spreading. To trigger a pandemic, the virus has to learn how to spread efficiently from person to person. Now that the genome of the 1918 virus has been completely sequenced, we understand that it may have taken only a few dozen mutations to turn a bird flu virus into humanity’s greatest killer, and we have seen some of those changes taking form in H5N1. The further H5N1 spreads and the more people it infects, the greater the likelihood that it might lock in mutations that could allow for efficient human-to-human transmission. “And that’s what keeps us up at night,” said the chair of the Infectious Diseases Society of America’s task force on pandemic influenza.
How Did Bird Flu Emerge?
More than a century ago, researchers confirmed the first outbreak of a particularly lethal form of avian influenza that they called “fowl plague.” Plague comes from the Greek word meaning “blow” or “strike.” Later, the name “fowl plague” was abandoned and replaced by “highly pathogenic avian influenza” or HPAI.
Domesticated poultry can also become infected with a low-grade influenza, so-called low pathogenic avian influenza, or LPAI, which may cause a few ruffled feathers and a drop in egg production. Influenza viruses with H5 or H7 spikes, however, are able to mutate into the high-grade variety that can cause devastating illness among the birds. Webster’s term for H5 and H7 strains of flu says it all: “the nasty bastards.” And you don’t get nastier than H5.
Avian Influenza, Poultry, and Eggs
To avoid contracting bird flu, an influenza expert at the UK Health Protection Agency warned, “[a]void being in touching distance [of birds who could be affected]. Don’t kiss chickens.” Kissing aside, what is the risk of putting our lips on them in other ways?
In 2001, the virus was found and confirmed in frozen duck meat. The investigators concluded, “The isolation of an H5N1 influenza virus from duck meat and the presence of infectious virus in muscle tissue of experimentally infected ducks raises concern that meat produced by this species may serve as a vehicle for the transmission of H5N1 virus to humans.”
The finding of H5N1-contaminated poultry meat triggered a more extensive survey. Top flu researchers at the U.S. Department of Agriculture (USDA) looked into chicken meat. Chickens who inhaled H5N1 became infected even more systemically than did ducks. The virus spread through the internal organs, into the muscle tissue, and even out into the skin. Virus was found in both white and dark meat.
There is a precedent for bird-borne virus-infected meat. Unlike bacteria, viruses can remain infective for prolonged periods even in processed foods. Some methods of preservation, like refrigeration, freezing, or salting, may even extend the persistence of viruses in food. On the other hand, since viruses cannot replicate without living tissue, improper storage of food is less problematic.
What about eggs? “Be careful with eggs,” the World Health Organization has warned. “Eggs from infected poultry could also be contaminated with the [H5N1] virus…”
Mutating and Getting More Virulent
Within a single individual, a virus evolves, adapts, learns. It hits dead ends and tries something new, slowly notching up mutations that may lock into place the ability to effectively survive in, and transmit between, people. Every single person who gets infected presents a risk of spawning the pandemic virus. Describes one virologist, “You’re playing Russian roulette every time you have a human infection.” Experts fear that as more and more people become infected, a virus will finally figure out the combination—the right combination of mutations to spread not just in one elevator or building, but in every building, everywhere, around the globe. Then it won’t just be peasant farmers in Vietnam dying after handling dead birds or raw poultry—it will be New Yorkers, Parisians, Londoners, and people in every city, township, and village in the world dying after shaking someone’s hand, touching a doorknob, or simply inhaling in the wrong place at the wrong time. It’s happened before, and it may soon happen again.
Said a WHO spokesperson about a virus like H5N1, “All the indications are that we are living on borrowed time.” A senior associate at the Center for Biosecurity listed the indications: “The lethality of the virus is unprecedented for influenza, the scope of the bird outbreak is completely unprecedented and the change that needs to happen to create a pandemic is such a small change—it could literally happen any day.”
Never before H5N1 had bird flu spread so far, so fast, and the longer the virus circulates in poultry production systems the higher the likelihood of additional human exposure.
Can H5N1 Be Eradicated?
H5N1 may be here to stay. “This virus cannot now be eradicated from the planet,” said Center for Biosecurity director O’Toole. “It is in too many birds in too many places.” The virus seemed to be getting more entrenched. “If you described it as a war, we’ve been losing more battles than we’ve won,” a WHO spokesperson told The Financial Times. “From a public health point of view, and an animal health point of view, this virus is just getting a stronger and stronger grip on the region.”
In a tone uncharacteristic of international policy institutions, the FAO wrote: “Over this bleak landscape sits a black cloud of fear that the virus might become adapted to enable human-to-human transmission and then spread around the globe.” The urgency and alarm among those tracking H5N1’s building momentum was palpable. “It’s like watching a volcano getting ready to erupt,” described a spokesperson of the World Organization for Animal Health (known as OIE, for Office Internationale des Epizooties). “We’re all holding our breath,” said Julie Gerberding, former head of the CDC.
Breeding Grounds for Disease
The world’s three leading authorities—the Food and Agriculture Organization of the United Nations, the World Health Organization, and the World Organization for Animal Health—held a joint consultation in 2004 to determine the key underlying causes. Four main risk factors for the emergence and spread of these diseases were identified. Bulleted first: “Increasing demand for animal protein.” This has led to what the CDC refers to as “the intensification of food-animal production,” the factor blamed in part for the increasing threat.
The way we kept animals when we first domesticated them ten thousand years ago is a far cry from how they are reared today. Chickens used to run around the barnyard on small farms. Now, “broiler” chickens—those raised for meat—are typically warehoused in long sheds confining an average of 20,000 to 25,000 birds. A single corporation, Tyson, can churn out more than 20 million pounds of chicken meat a day. Worldwide, an estimated 70 to 80 percent of egg-laying chickens are intensively confined in battery cages, small barren wire enclosures stacked several tiers high and extending down long rows in windowless sheds. The cages are stocked at such densities that each hen is typically allotted less floor space than a standard letter-sized piece of paper. It is not uncommon for egg producers to keep hundreds of thousands—or even a million—hens confined on a single farm. Half the world’s pig population—now approaching one billion—is also crowded into industrial confinement operations. This represents the most profound alteration of the animal-human relationship in ten thousand years.
What Can We Do?
To reduce the emergence of viruses like H5N1, humanity must shift toward raising birds in smaller flocks, under less stressful, less crowded, and more hygienic conditions, with outdoor access, no use of human antivirals, and with an end to the practice of breeding for rapid growth or unnatural egg production at the expense of immunity. This would also be expected to reduce rates of increasingly antibiotic-resistant pathogens such as Salmonella, the number one foodborne killer in the United States. We need to move away from the industry’s fire-fighting approach to infectious disease to a more proactive preventive health approach that makes birds less susceptible—even resilient—to disease in the first place.
In the United States, the American Public Health Association (APHA) is among those advocating for “radical” (from the Latin radix, for “root”) change. In 2003, the APHA passed a “Precautionary Moratorium on New Concentrated Animal Feed Operations,” in which it urged all federal, state, and local authorities to impose an immediate moratorium on the building of new factory farms—including industrial turkey, laying hen, broiler chicken, and duck facilities. In November 2019, it reiterated its stance, publishing a new policy statement calling once again for a moratorium on new factory farms, as well as a moratorium on the expansion of existing ones.
Eating to Beat Bird Flu
The journal of the APHA published an editorial entitled “The Chickens Come Home to Roost” that went beyond just calling for a deintensification of the pork and poultry industries. The editorial questioned the prudence of raising so many animals for food in the first place, given the pandemic threat they may pose: “It is curious, therefore, that changing the way humans treat animals, most basically ceasing to eat them, or at the very least, radically limiting the quantity of them that are eaten—is largely off the radar as a significant preventive measure. Such a change, if sufficiently adopted or imposed, could still reduce the chances of the much-feared influenza epidemic. It would be even more likely to prevent unknown future diseases that, in the absence of this change, may result from farming animals intensively and killing them for food. Yet humanity doesn’t even consider this option.”
However, thanks to food innovations, this may be changing, with plant-based meats, milks, and eggs growing in popularity with expanded options in supermarkets. And, making healthier choices could also help mediate the next coronavirus epidemic by also decreasing the rates of comorbidities found to increase the risk in SARS, MERS, and COVID-19. For example, consider the underlying risk factors for COVID-19 severity and death—obesity, heart disease, hypertension, and type 2 diabetes—all of which can be controlled or even reversed with a healthy enough plant-based diet and lifestyle.
Egg-Free Eggs
There are so many delicious egg-free egg recipes, like this Garden Veggie Tempeh Scramble created by NutritionFacts.org’s own executive director.
Conclusion
H5N1 was discovered in chickens decades ago, a flu virus that would forever change our understanding of how bad pandemics could get—a flu virus that appears capable of killing half the people it infects. Imagine if a virus like that started explosively spreading from human to human. Consider a pandemic a hundred times worse than COVID-19, one with a fatality rate not of one in two hundred but rather a coin flip of one in two. Thankfully, H5N1 has so far remained a virus mainly of poultry, not people, but H5N1 and other new and deadly animal viruses like it are still out there, still mutating, with an eye on the eight-billion-strong buffet of human hosts. With pandemics, it’s never a matter of if, but when. A universal outbreak with more than a few percent mortality wouldn’t just threaten financial markets but civilization itself as we know it.
A pandemic triggered by a bird flu virus could leave hundreds of millions dead. “An influenza pandemic of even moderate impact,” Michael Osterholm, the director of the Center for Infectious Disease Research and Policy at the University of Minnesota, wrote, “will result in the biggest single human disaster ever—far greater than AIDS, 9/11, all wars in the 20th century and the recent tsunami combined. It has the potential to redirect world history as the Black Death redirected European history in the 14th century.”1 Hopefully, for humanity’s sake, the direction world history will take is away from raising birds by the billions under intensive confinement so as to potentially lower the risk of us ever being in this same precarious place in the future. The silver lining of COVID-19 is that the world will be better prepared for the next global health crisis. Tragically, it may take a pandemic with a virus like H5N1 before the world realizes the true cost of cheap chicken.
1 Kennedy M. 2005. Bird flu could kill millions: global pandemic warning from WHO. “We’re not crying wolf. There is a wolf. We just don’t know when it’s coming.” Gazette (Montreal), March 9, p. A1.
May 1, 2025
Inhospitable Hospital Food
What do hospitals have to say for themselves about serving meals that appear to be designed to inspire repeat business?
“Hospital food needs a revolution.” I was surprised to learn that most inpatient meals served in hospitals are “not required to meet national nutrition standards for a healthy diet.” An analysis of the nutritional value of food served to patients in teaching hospitals found that many did not meet dietary recommendations. “Warning: Hospital food bad for health,” read the headline.
A registered dietitian wrote to defend hospitals and point out how stringent the guidelines are, saying that “over half the hospitals met or exceeded more than half the guidelines….It would not take more than choosing eggs for breakfast and 2 percent milk with meals to exceed the recommended intake of cholesterol and fat…The provocative conclusions of Singer et al. only lead the media and the public to conclude that we are a bunch of dunces who have no understanding of the relation between nutrition and disease prevention.”
Well, if the white coat fits…
“We spend a fortune on training doctors, but then don’t follow through on the simplest things, like food.” “Good diet is as necessary to recovery of health as good nursing, surgery, or medicine, and it is folly to pretend that it is beyond the power of our profession to change this reproach.” That was written 75 years ago, yet still there is pushback: “Perhaps we should question whether a ‘healthy diet’ given to a helpless patient during a 2- to 10-day hospital stay benefits anyone or anything other than the dietitian’s sense of ‘doing good,’” responded one doctor. He added, “I am always bothered when a healthy 75-year-old…is deprived of a desired morning egg because a ‘healthy’ low-cholesterol diet has been ordered.” I mean, what is a few days of a little heart-unfriendly diet in the scheme of things…
But it’s the message that’s being sent. “The presence of foods on the [hospital] tray sends a message to patients as to what is healthy and acceptable for them to eat,” responded the researchers who did the hospital foods analysis. “We still can think of no better place or opportunity to set an example of good nutrition than when patients are in hospitals.”
After all, public schools in California, for instance, have banned the sale of sodas for more than a decade. Why not children’s hospitals? In a study of California healthcare facilities serving children, 75 percent of beverages and 81 percent of foods sold in vending machines wouldn’t have been allowed to be sold in schools. We’re talking soda and candy. “Having unhealthy items in health care facilities and seeing staff consume these products…contradicts the nutrition and health messages children often receive from health care providers.”
On adult menus, nearly all meals contained excess salt, with 100 percent of daily menus exceeding the American Heart Association’s recommendation for staying under 1,500 mg of sodium a day. This means meals offered to patients may actually “contribute to the exacerbation or slow resolution of the very conditions that may have led to the hospitalization,” as I discuss in my video Just How Bad Is Hospital Food?.
But if hospitals adhered to the recommended limits of salt, the food wouldn’t taste as good, responded an executive from the Salt Institute, to which the researchers replied: Taste as good? “Hospital food is often criticized as having poor palatability, despite the fact that it likely already contains high levels of sodium.” It doesn’t taste good, no matter how much salt it has.
At the very least, we should “prepare all meals with low sodium content and make optional table salt available for those patients who do not have additional restrictions.” Then, if individuals want to add salt, it’s their choice. If they want to get someone to wheel them out into the parking lot and smoke, that’s their business, but we shouldn’t be blowing cigarette smoke into patients’ rooms three times a day, whether they want it or not. Interestingly, studies suggest that when people are allowed to salt food to taste, they rarely add as much sodium as may come in prepackaged foods.
As you can see below and at 3:55 in my video, when researchers switched study participants to a low-sodium diet, they used their saltshakers more, but, overall, their salt intake dipped way down. And they said their food tasted just as salty, because salt added to the surface of foods makes it taste saltier. But when a hospital meal is served pre-salted, “most inpatients may not actually have the option to consume healthy levels of sodium while they are hospitalized.”

In defense of their unhealthy food, one hospital food service provider explained that they’re just giving people what they want: “People are in the hospital and they are stressed and they need something that they consider comfort food, so I don’t want to deny that to people if that’s what makes them feel better.” That’s a reason one clinical director sends ice cream and candy bars to cancer patients: “We focus on familiar comfort foods, an approach that has enhanced patient satisfaction and improved intake.” You know what else might help? A nice, long drag on a cigarette. Hospitals used to sell cigarettes, “primarily…for ‘patient convenience.’” “‘I don’t think I can deny a paying patient the right to smoke a cigarette,’” said a medical center administrator. “‘As a service to the patient, I will have to insist we have cigarette machines in the hospital.” But others suggested that tobacco products shouldn’t be sold in hospitals at all. This wasn’t from the 1950s, but from the 1980s. Yet, at the time, the “irony of hospitals allowing the sale of cigarettes, which are the major cause of preventable illness and death in this country, has rarely been discussed in the literature…It is especially ironic that smoking is permitted in 89% of doctors’ lounges.”
To their credit, though, U.S. hospitals underwent “the first industry-wide ban on smoking in the workplace” by the mid-1990s. Now, “hospitals again have the opportunity to take the lead and to create food environments that are consistent with their mission to cure the sick and to promote health. Through the simple act of serving food that meets national nutritional standards, our hospitals will act in the best health interests of their patients, and their staff, and will undoubtedly again be leaders in our ongoing dialogue on how to improve our food supply, which in turn will improve the health of us all.”
“Strict antismoking regulations have frequently been criticized as too harsh or difficult to enforce, as if disease and premature death brought on by smoking were any easier to accept and control.” Think my smoking-diet parallel is hyperbole? Well, guess what? Today, the major cause of preventable illness and death in this country is no longer tobacco. The leading cause of death in America is now the American diet, as shown below and at 6:29 in my video. Hospitals in the United States serve “millions of patient meals each day and are optimally positioned to model a healthy diet through patient food.”

Doctor’s Note:
Have you seen my earlier video on junk food in hospitals? If not, check out Hospitals’ Profit on Junk Food.
For more on how the profit motive is degrading our health, see related posts below.