Michael Greger's Blog, page 10
November 14, 2024
A Look at Bariatric Surgery
Obesity isn’t new, but the obesity epidemic is. We went from a few corpulent queens and kings, like Henry VIII and Louis VI (known as Louis le Gros, or “Louis the Fat”), to a pandemic of obesity, now considered to be perhaps the direst and most poorly contained public health threat of our time. Today, 71 percent of American adults are overweight and 40 percent of men and women appear to have so much body fat that they can be classified as obese, and there’s no end in sight.
In 2013, the American Medical Association voted to classify obesity as a disease against the advice of its own Council on Science and Public Health. Disease implies dysfunction, but bariatric drugs and surgery are not fixing physiological malfunction. Our bodies are just doing what they were designed to do in the face of excess calories. Rather than some sort of disorder, weight gain may largely be a normal response, by normal people, to an abnormal situation. And with more than 70 percent of Americans now overweight, it’s literally normal.
What Is Bariatric Surgery?
Bariatric surgeries involve changing our digestive system to facilitate weight loss. As discuss in my video The Mortality Rate of Bariatric Weight Loss Surgery, the use of bariatric surgery has exploded from about 40,000 procedures, noted in the first international survey in 1998, to now hundreds of thousands performed every year in the United States alone. The first technique developed, the intestinal bypass, involved carving out about 19 feet of intestines.
The most common procedure is stomach stapling, also known as sleeve gastrectomy, in which most of the stomach is permanently removed. Only a narrow tube of stomach is left, so as to restrict how much food can be eaten at any one time. Bariatric surgery can be thought of as a form of internal jaw wiring.
Gastric bypass, known as Roux-en-Y gastric bypass, is the second most common bariatric surgery. It combines restriction—stapling the stomach into a pouch smaller than a golf ball—with malabsorption by rearranging our anatomy to bypass the first part of our small intestine. It appears to be more effective than just cutting out most of the stomach. It results in a loss of about 63 percent of excess weight, compared to 53 percent with a gastric sleeve.
After sleeve gastrectomy and Roux-en-Y gastric bypass, the third most common bariatric procedure is a revision to fix a previous bariatric procedure.
Is Weight Loss Sustainable After Bariatric Surgery?
As discussed in my video How Sustainable Is the Weight Loss After Bariatric Surgery, bariatric surgery may result in weight loss, but most patients end up regaining some of the fat they lose over the first year or two after surgery, but five years later, three-quarters maintain at least a 20 percent weight loss.
The typical trajectory for someone who starts out obese at 285 pounds, for example, would be to drop to an overweight 178 pounds two years after bariatric surgery, but then regain back up to an obese 207 pounds. This has been chalked up to “grazing” behavior, where compulsive eaters may shift from bingeing, which becomes more difficult post-surgery, to eating smaller amounts constantly throughout the day. Eight years out, about half of gastric bypass patients continue to describe episodes of disordered eating. As one pediatric obesity specialist described, “I have seen many patients who put chocolate bars into a blender with some cream, just to pass technically installed obstacles” [like a gastric band].
Does Bariatric Surgery Cure Diabetes?
As I discuss in my video Bariatric Surgery vs. Diet to Reverse Diabetes, after bariatric surgery, about 50 percent of individuals with diabetes and obesity, as well as 75 percent with diabetes and super-obesity, go into remission, meaning they have normal blood sugars on a regular diet off all diabetes medications. Are we sure it was the surgery, though?
At a bariatric surgery clinic at the University of Texas, patients with type 2 diabetes scheduled for a gastric bypass volunteered to first undergo an identical period of caloric restriction, but without the surgery. They were placed in the hospital and put on the same diet they would be on immediately before and after the surgery for ten days, averaging less than 500 calories a day to mimic the surgical situation. Then, the researchers waited a few months so the patients would gain back the weight and then put them through the actual surgery, matched day-for-day to the diets they were on before. So, the same patients and the same diets, just with or without the actual surgery.
If there were some sort of metabolic benefit to the anatomical rearrangement, they would have done better after the actual surgery, but in some ways they actually did worse. The caloric restriction alone resulted in similar improvements in blood sugar, pancreatic function, and insulin sensitivity, but several measures of diabetic control improved significantly more without the surgery. So, the surgery seemed to put them at a metabolic disadvantage.
The caloric restriction works by first mobilizing fat out of the liver. Type 2 diabetes is thought to be caused by fat building up in the liver, which then spills over into the pancreas. Everyone may have a “personal fat threshold” for the safe storage of excess fat. When that limit is exceeded, fat gets deposited in the liver, where it causes insulin resistance. The liver attempts to offload some of the fat, which then gets stuck in the pancreas, and can kill off the cells that produce insulin. By the time diabetes is diagnosed, half of our insulin-producing cells may have been destroyed. Put people on a low-calorie diet, though, and this entire process can be reversed.
A large enough negative caloric balance can cause a profound drop in liver fat sufficient to resurrect liver insulin sensitivity within seven days. Keep it up, and the liver stops spitting out fat enough to help normalize pancreatic fat levels and function within just eight weeks. Once you drop below your personal fat threshold, you should then be able to resume normal intake and still keep your diabetes at bay. The bottom line is that type 2 diabetes is reversible with weight loss, if you catch it early enough.
Reasons Not to Have Bariatric Surgery
More than 30,000 intestinal bypass operations were performed before “catastrophic,” “disastrous outcomes” were recognized. This included protein deficiency-induced liver disease, which often progressed to liver failure and death. This inauspicious start is remembered as “one of the dark blots in the history of surgery.”
Today, death rates after bariatric surgery are considered “very low,” occurring on average in perhaps 1 in 300 to 1 in 500 patients. But gastric bypass carries a greater risk of serious complications. Many are surprised to learn that new surgical procedures don’t require premarket testing or, in the United States, for instance, Food and Drug Administration approval, and they are largely exempt from rigorous regulatory scrutiny.
What’s more, up to 25 percent of bariatric patients have to go back into the operating room for problems caused by their first bariatric surgery, as discussed in my video The Complications of Bariatric Weight-Loss Surgery. And re-operations are riskier, carrying around ten times the mortality rate, and offer no guarantee of success. Complications include leaks, fistulas, ulcers, strictures, erosions, obstructions, and severe acid reflux.
Gastric bypass is such a complicated procedure that the learning curve may require 500 cases for a surgeon to master the procedure. Complications risk plateaus after about 500 cases, with the lowest risk found among surgeons who’ve performed more than 600 bypasses. The risk of not making it out alive may be double under the knife of those who’ve done less than 75, compared to more than 450. So, if you do choose to undergo the operation, I’d recommend asking your surgeon how many procedures they’ve done, as well as choosing an accredited bariatric “Center of Excellence,” where surgical mortality appears to be two to three times lower than non-accredited institutions.
Even if the surgical procedure goes perfectly, lifelong nutritional replacement and monitoring are required to avoid vitamin and mineral deficits. This includes more than a little anemia, osteoporosis, or hair loss, but full-blown cases of life-threatening deficiencies, such as beriberi, pellagra, kwashiorkor, and nerve damage, which can manifest as vision loss years or even decades after surgery in the case of copper deficiency. Tragically, in cases of severe deficiency of a B vitamin called thiamine, nearly one in three patients progressed to permanent brain damage before the condition was caught.
The malabsorption of nutrients is on purpose for procedures like gastric bypass. By cutting out segments of the intestines, you can successfully impair the absorption of calories, but at the expense of impairing the absorption of necessary nutrition. Even people who just undergo restrictive procedures like stomach stapling can be at risk for life-threatening nutrient deficiencies because of persistent vomiting. Indeed, vomiting is reported by up to 60 percent of patients after bariatric surgery due to “inappropriate” eating behaviors (in other words, trying to eat normally). The vomiting helps with weight loss similar to the way a drug for alcoholics called Antabuse can be used to make them so violently ill after a drink that they eventually learn their lesson.
“Dumping syndrome” can work the same way. A large percentage of gastric bypass patients can suffer from abdominal pain, diarrhea, nausea, bloating, fatigue, or palpitations after eating calorie-rich foods as they bypass your stomach and dump straight into the intestines. As surgeons describe it, this is a feature, not a bug: “Dumping syndrome is an expected and desired part of the behavior modification caused by gastric bypass surgery; it can deter patients from consuming energy-dense food.”
Colorectal cancer appears to be the only malignancy for which the risk goes up after obesity surgery. After bariatric surgery, the rate of rectal cancer death may triple. The rearrangement of anatomy involved in one of the most common surgeries—gastric bypass—is thought to increase bile acid exposure along the intestinal lining. This causes sustained pro-inflammatory changes even years after the procedure, which are thought to be responsible for the increased cancer risk. In contrast, losing weight by dietary means has the potential to decrease obesity-related cancer risk across the board.
Bariatric Surgery and Mental Health
As you can imagine, weight regain after surgery can have devastating psychological effects, as patients may feel they failed their last resort. This may explain why bariatric surgery patients are at a high risk of depression and suicide.
Now, severe obesity alone may increase risk of suicidal depression, but even at the same weight, those going through surgery appear to be at higher risk. At the same BMI, age, and gender, bariatric surgery recipients have nearly four times the odds of suicide compared with counterparts not undergoing the procedure. Most convincingly, before-and-after mirror-image analyses show the risk of serious self-harm increases post-surgery among the same individuals.
About 1 in 50 bariatric surgery patients end up killing themselves or being hospitalized for self-harm or attempted suicide, and this only includes confirmed suicides, excluding masked attempts such as overdoses of “undetermined intention.” Bariatric surgery patients also have an elevated risk of accidental death, though some of this may be due to changes in alcohol metabolism. Give gastric bypass patients two shots of vodka, and because of their altered anatomy, their blood alcohol level shoots up past the legal driving limit within minutes. It’s unclear whether this plays a role in the 25 percent increase in prevalence of alcohol problems noted during the second postoperative year.
Even those who successfully lose their excess weight and keep it off appear to have a hard time coping. Ten years out, although physical health-related quality-of-life improves, general mental health tends to significantly deteriorate, compared to pre-surgical levels even among the biggest losers. Ironically, there’s a common notion that bariatric surgery is for “cheaters” who take the easy way out by choosing the “low-effort” method of weight loss.
Shedding the pounds may not shed the stigma of even prior obesity. Studies suggest that in the eyes of others, knowing someone was fat in the past leads them to always be treated more like a fat person. And there’s a strong anti-surgery bias on top of that, such that those who choose the scalpel to lose weight are rated most negatively (for example, being considered less physically attractive). One can imagine how remaining a target of prejudice even after joining the “in-group” could potentially undercut psychological well-being.
Who Is a Good Candidate for Bariatric Surgery?
A body gaining weight when excess calories are available for consumption is behaving as it should. Efforts to curtail such weight gain with drugs or surgery are not efforts to correct an anomaly in human physiology but rather to deconstruct and reconstruct its normal operations at the core. Critics have pointed out this irony of surgically altering healthy organs to make them dysfunctional (“malabsorptive”) on purpose, especially when it comes to operating on children. Bariatric surgery for kids and teens is becoming widespread and performed on children as young as five years old. Surgeons defend the practice by arguing that growing up fat can leave emotional scars and “lifelong social retardation.”
Promoters of preventive medicine argue that bariatric surgery is the proverbial “ambulance at the bottom of the cliff.” In response, a proponent of pediatric bariatric surgery said, “It is often pointed out that we should focus on prevention. Of course, I agree. However, if someone is drowning, I don’t tell them, ‘You should learn how to swim’; no, I rescue them.”
A strong case can be made that the benefits of bariatric surgery far outweigh the risks if the alternative is remaining morbidly obese, which is estimated to shave off up to 13 years of one’s life. Although there are no data from randomized trials yet to back it up, compared to obese individuals who hadn’t been operated on, those getting bariatric surgery would be expected to live significantly longer on average. It’s no wonder surgeons consistently frame the elective surgery as a life-or-death necessity, but the benefits only outweigh the risks if there are no other alternatives.
False Advertising
Bariatric surgery advertising is filled with happily-ever-after fairytale narratives of cherry-picked outcomes offering, as one ad analysis put it, “the full Cinderella-romance happy ending.” This may contribute to the finding that patients often overestimate the amount of weight they’ll lose with the procedure and underestimate the difficulty of the recovery process. Surgery forces profound changes in eating habits, requiring slow, thoroughly chewed, small bites. Your stomach goes from the volume of two softballs down to the size of half a tennis ball in stomach stapling, and half a ping-pong ball in the case of gastric bypass or banding.
“Even if surgery proves sustainably effective,” wrote the founding director of Yale University’s Prevention Research Center, “the need to rely on the rearrangement of our natural gastrointestinal anatomy as an alternative to better use of feet and forks”—that is, exercise and diet—“seems a societal travesty.”
Might there be a way to lose weight healthfully without resorting to the operating table? Yes, a whole food, plant-based diet.
November 11, 2024
Celebrating Veterans Day with Bill Muir
We had the pleasure of talking with Bill Muir about his work in the military and as a Registered Nurse, food access, his book, and Veterans Day. We hope you enjoy this interview.

Thank you for your service. We are grateful for the opportunity to interview you. Please tell us about yourself and your background. Why did you decide to join the military, and when did you enlist?
Thank you very much! Hi, everyone. I’m Bill Muir, aka SGT VEGAN. I’m a combat veteran, RN, and 32-year vegan. I joined the U.S. Army after 9/11 to serve my country in its time of need. I had been living in Japan for about eight years at the time the attack happened, and, as an expat, it affected me very deeply. I joined the military because I thought I would be able to make a difference and help save lives, both American and Afghan, if I joined during war.
What branch of the military were you in? What was your job? Where did you serve?
I was a U.S. Army Paratrooper and served with the 173rd Airborne Brigade as a combat medic. I did a tour in Afghanistan from 2005 to 2006.
What was your experience like eating a plant-based diet while serving? Did you experience particular challenges with food access? If so, how did you overcome them?
Being vegan in the military really depends on where you are and what you are doing. Basic training was completely awful––not because training was hard, but because I was starving all the time. After bootcamp, things got better and I put the weight back on. Being stationed in Italy with the 173rd was amazing! I actually got kind of fat despite all the running I was doing, because I was eating vegan pasta, vegan pizza, and vegan gelato every day. When I deployed, I was very worried I would go back to starvation mode, but, luckily, I found a website called anysoldier.com that sends deployed service people what they need. I’ve heard conditions for people on plant-based diets have gotten better, but until there are designated vegan MRES (field rations) and plant-based options in all military cafeterias, it will be difficult to be plant-based in the military.
Why was it important to you to remain plant-based during your military career?
To me, being vegan meant living my ethics. I think remaining true to something I believe in while in the military, especially while in a warzone, was also about my attempt to hold on to my identity.
How did your time in the military shape who you are today? Is there anything in particular about your service that you would like to share?
No matter who you are, being in the military will change you almost down to a cellular level. I know that’s a popular trope in every movie and TV show featuring the military, but somehow I wasn’t expecting that would include me as well.
After your military service, you earned a certificate in Vegan Culinary Arts from Atlantic Union College. In your opinion, how can education about preparing whole plant foods be a path forward for people to achieve better health?
It can be huge, but people have to want to change. A vast majority of my patients have checked out and given up on trying to be healthy. I’m just trying to do the best I can to keep them from falling or dying on my shift. There is still a lot of anti-vegan propaganda in the United States, and, unfortunately, a lot of veterans still believe that somehow eating dead animals makes you more masculine.
After you transitioned out of the military, you became a Registered Nurse. What has your experience been like working in the medical field and what area of nursing is your specialty?
Working for Veterans Affairs (VA) as an RN has been both a blessing and a curse. On one hand, I feel lucky to be able to help my fellow veterans in their time of need, in much the same way as I joined the military in a time of war. On the other hand, working with sick and dying people takes its toll on you both physically and mentally. All in all, I feel lucky to have a job doing something that matters, but sometimes I wish I had chosen an easier profession.
Do you still work for a VA hospital? Have you seen conditions that could be preventable with healthy lifestyle interventions, like whole food, plant-based eating?
I work on a VA Medical/Surgical floor that has heart monitors. The vast majority of cardiac issues are lifestyle-related, meaning the patients’ hearts aren’t working the way they should because of unhealthy diets, smoking, drinking, or drugs. While we can’t live forever, we can live better, longer, if we just make simple lifestyle adjustments. The top three? Go vegan, exercise daily, and don’t smoke.
Please tell us about your book
Vegan Strong
. What inspired you to write it?
After I went to culinary school, I planned to open a restaurant. Unfortunately, my timing wasn’t great. It was 2008 and the economy was on the rocks, so I shelved that dream and made the practical choice to become a Registered Nurse. I didn’t know what I was going to do with all of my knowledge of plant-based health and plant-based living until, one day, I had an idea. I would write a book about how to be healthy and vegan, but style it like an Army Field Manual.
Lastly, what does Veterans Day mean to you? Is there anything you would like to share with your fellow veterans?
Veterans Day is our day, so as a veteran, if you want it to be about getting some free meals, go for it. If you want it to be about meaningful reflection, that’s cool, too. We are around 6 percent of the population, and if you served during wartime, that number is even smaller. Eat right, take care of yourself, and if you need help, the VA is always there for you. GO VEGAN AND STAY VEGAN STRONG!
For more information about my work and latest updates, visit my website and follow me on social media at IG @sgt_vegan, and Facebook.
November 7, 2024
Drinking Water, Losing Weight
A few times a day, drink two cups of cold water on an empty stomach for weight loss.
After drinking two cups (half a liter) of water, you can get a surge of the adrenal hormone noradrenaline in your bloodstream, as if you had just smoked a few cigarettes or had a few cups of coffee, boosting your metabolic rate up to 30 percent within an hour, as shown below and at 0:22 in my video Optimizing Water Intake to Lose Weight. When put to the test in randomized controlled trials, that appeared to accelerate weight loss by 44 percent, making drinking water the safest, simplest, and cheapest way to boost your metabolism.

Now, this entire strategy may fail if you’re on a beta-blocker drug. (Beta blockers are typically prescribed for heart conditions or high blood pressure and tend to end with the letters lol, such as atenolol, nadolol, or propranolol, sold as Tenormin, Corgard, or Inderal, respectively.) So, for example, as you can see below and at 0:59 in my video, if you give people the beta-blocker drug metoprolol (sold as Lopressor) before they drink their two cups (480 mL) of water, the metabolic boost is effectively prevented. This makes sense since the “beta” being blocked by beta blockers are the beta receptors triggered by noradrenaline. Otherwise, drinking water should work. But what’s the best dose, type, temperature, and timing?

Just a single cup (240 mL) of water may be sufficient to rev up the noradrenaline nerves, but additional benefit is seen with drinking two or more cups (480 mL). A note of caution: One should never drink more than about three cups (710 mL) in an hour, since that starts to exceed the amount of fluid your kidneys can handle. If you have heart or kidney failure, your physician may not want you to drink extra water at all, but even with healthy kidneys, any more than three cups of water an hour can start to critically dilute the electrolytes in your brain with potentially critical consequences. (In How Not to Diet, I talk about a devastating, harrowing experience I had in the hospital as an intern. A patient drank himself to death—with water. He suffered from a neurological condition that causes pathological thirst. I knew enough to order his liquids to be restricted and have his sink shut off, but I didn’t think to turn off his toilet.)
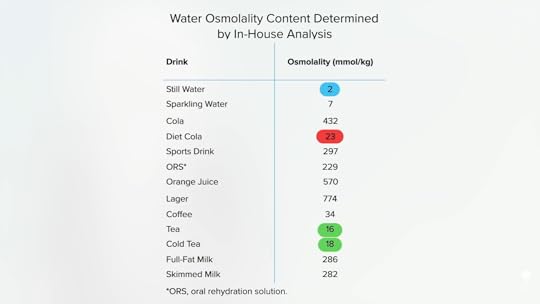
Getting back to it. What kind of water are we talking about? Does it have to be plain, regular water? It shouldn’t matter, right? Isn’t water just water whether it’s flavored or sweetened in a diet drink? Actually, it does matter. When trying to prevent fainting before blood donation, drinking something like juice doesn’t work as well as plain water. When trying to keep people from getting dizzy when they stand up, water works, but the same amount of water with salt added doesn’t, as seen below and at 2:40 in my video. What’s going on?

We used to think the trigger was stomach distention. When we eat, our body shifts blood flow to our digestive tract, in part by releasing noradrenaline to pull in blood from our limbs. This has been called the gastrovascular reflex. So, drinking water was thought to be a zero-calorie way of stretching our stomachs. But, instead, if we drink two cups (480 mL) of saline (basically salt water), the metabolic boost vanishes, so stomach expansion can’t explain the water effect.
We now realize our body appears to detect osmolarity, the concentration of stuff within a liquid. When liquids of different concentrations were covertly slipped into people’s stomachs via feeding tubes, detection of plain water versus another liquid was demonstrated by monitoring sweat production, which is a proxy for noradrenaline release. It may be a spinal reflex, as it’s preserved in people who are quadriplegic, or picked up by the liver, as we see less noradrenaline release in liver transplant patients (who’ve had their liver nerves severed). Whichever the pathway, our body can tell. Thought we only had five senses? The current count is upwards of 33.
In my Daily Dozen recommendation, I rank certain teas as among the healthiest beverages. After all, they have all the water of water with an antioxidant bonus. But, from a weight-loss perspective, plain water may have an edge. That may explain the studies that found that overweight and obese individuals randomized to replace diet beverages with water lost significantly more weight. This was chalked up to getting rid of all those artificial sweeteners, but, instead, it may be that the diet drinks were too concentrated to offer the same water-induced metabolic boost. As you can see below and at 4:29 in my video, diet soda, like tea, has about ten times the concentration of dissolved substances compared to tap water. So, plain water on an empty stomach may be the best.
Does the temperature of the water matter? In a journal published by the American Society of Mechanical Engineers, an engineering professor proposed that the “secret” of a raw food diet for weight loss was the temperature at which the food was served. “Raw food, by its very nature, is consumed at room temperature or lower.” To bring two cups (480 mL) of room-temperature water up to body temperature, he calculated the body would have to dip into its fat stores and use up 6,000 calories. Just do the math, he says: A calorie is defined as the amount of energy required to raise one gram of water one degree Celsius. So, since two cups of water are about 500 grams and the difference between room temp and body temp is about a dozen degrees Celsius, it’s about 500 x 12 = 6,000 calories needed.
Do you see the mistake? In nutrition, a “calorie” is actually a kilocalorie, a thousand times bigger than the same word used in the rest of the sciences. Confusing, right? Still, I’m shocked that the paper was even published.
So, drinking two cups of room-temperature water actually takes only 6 calories to warm up, not 6,000. Now, if you were a hummingbird drinking four times your body weight in chilly nectar, you could burn up to 2 percent of your energy reserves warming it up, but it doesn’t make as much of a difference for us.
What about really cold water, though? A letter called “The Ice Diet” published in the Annals of Internal Medicine estimated that eating about a quart (1 L) of ice—like a gigantic snow cone without any syrup—could rob our body of more than 150 calories, which is the “same amount of energy as the calorie expenditure in running 1 mile.” It’s not like you directly burn fat to warm up the water, though. Your body just corrals more of the waste heat you normally give off by constricting blood flow to your skin. How does it do that? Noradrenaline.
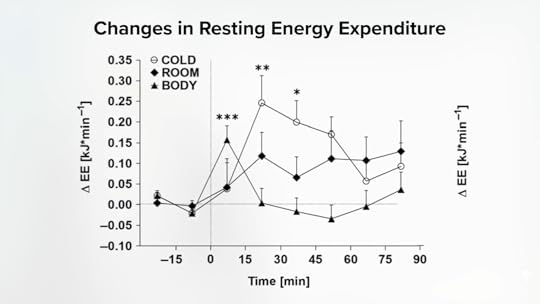
If you compare drinking body-temperature water, room-temperature water, and cold water, there’s only a significant constriction in blood flow to the skin after the room-temperature water and the cold water, as seen below and at 6:39 in my video.
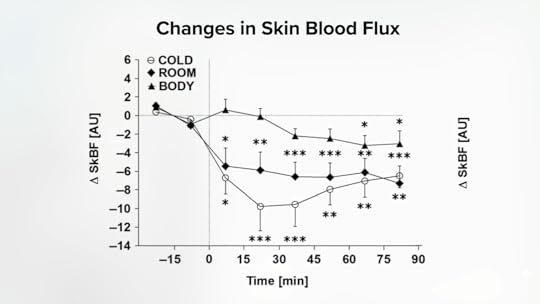
What’s more, as you can see here and at 6:45 in the video, neither the warm nor tepid water could boost metabolic rate as much as cold (fridge temperature) water. Our body does end up burning off more calories when we drink our water cold (at least indirectly).
So, two cups of cold water on an empty stomach a few times a day. Does it matter when? Yes, watch my Evidence-Based Weight Loss lecture to see how you can add the benefit of negative-calorie preloading by drinking that water right before your meals.
Too good to be true? No. Check out my other three videos on water and weight loss in the related posts below.
November 5, 2024
Boosting Your Metabolism Safely
If you drink two cups of water, the adrenal hormone noradrenaline can surge in your bloodstream, similar to the response of smoking a few cigarettes or having a few cups of coffee.
Given the 60 percent surge in noradrenaline within minutes of drinking just two cups of water, as shown in the graph below and at 0:13 in my video What Is the Safest Metabolism Booster?, might one be able to get the weight-loss benefits of noradrenaline-releasing drugs like ephedra—without the risks? You don’t know until you put it to the test. Published in the Journal of the Endocrine Society, the results were described as “uniquely spectacular.” Researchers found that drinking two cups of water increased the metabolic rate of men and women by 30 percent. The increase started within ten minutes and reached a maximum within an hour. In the 90 minutes after drinking one tall glass of water, the study participants burned about an extra 25 calories (100 kJ). Do that four times throughout the day, and you could eliminate 100 additional calories (400 kJ). That’s more than if you had taken ephedra! You’d trim off more calories drinking water than taking weight-loss doses of the banned substance ephedrine (the active component of ephedra) three times a day. And we’re just talking about plain, cheap, safe, and legal tap water.
Using the Ten-Calorie Rule I’ve explained previously, drinking that much water could make us lose ten pounds over time unless we somehow compensated by eating more or moving less. Concluded one research team, “In essence, water drinking provides negative calories.
A similar effect was found in overweight and obese children. Drinking about two cups of water led to a 25 percent increase in metabolic rate within 24 minutes, and it lasted at least 66 minutes, until the experiment ended. So, just getting the recommended daily “adequate intake” of water—about 7 cups (1.7 L) a day for children aged 4 through 8, and for ages 9 through 13, 8 cups (2.1 L) for girls and 10 cups (2.4 L) for boys, as shown below and at 1:45 in my video—may offer more than just hydration benefits.

Not all research teams were able to replicate these findings, though. For example, one found an increase of only about 10 to 20 percent, while another found only a 5 percent increase, and yet another team found effectively none at all. What we care about, though, is weight loss. The proof is in the pudding. Let’s test the waters, shall we?
Some researchers suggest that the “increase in metabolic rate with water drinking could be systematically applied in the prevention of weight gain….” Talk about a safe, simple, side-effect-free solution. It’s free in every sense. Drug companies may spend billions of dollars getting a new drug to market. Surely a little could be spared to test something that, at the very least, couldn’t hurt. That’s the problem, though. Drinking water is a “cost-free intervention.”
There are observational studies suggesting that those who drink four or more cups (1 L) of water a day, for example, appear to lose more weight, independent of confounding factors, such as drinking less soda or exercising more. What happens when you put it to the test?
In 2013, “Effect of ‘Water Induced Thermogenesis’ on Body Weight, Body Mass Index and Body Composition of Overweight Subjects” was published. Fifty “overweight girls”—who were actually women, aged 18 to 23—“were instructed to drink 500 ml [2 cups] of water, three times a day, half an hour before breakfast, lunch, and dinner, which was over and above their daily water intake” and without otherwise changing their diets or physical activity. The result? They lost an average of three pounds (1.4 kg) in eight weeks. What happened to those in the control group? There was no control group, a fatal flaw for any weight-loss study due to the “Hawthorne effect,” where just knowing you’re being watched and weighed may subtly affect your behavior. Of course, we’re just talking about drinking water. With no downsides, why not give it a try? I’d feel more confident if there were some randomized, controlled trials to really put it to the test. Thankfully, there are!
I hate it when the title ruins the suspense. “Water Consumption Increases Weight Loss During a Hypocaloric Diet Intervention in Middle-Aged and Older Adults.” Overweight and obese men and women randomized to two cups of water before each meal lost nearly five pounds more body fat in 12 weeks than those in the control group, as shown below and at 4:08 in my video. Both groups were put on the same calorie-restricted diet, but the one with the added water lost weight 44 percent faster.

A similar randomized controlled trial found that about 1 in 4 in the water group lost more than 5 percent of their body weight compared to only 1 in 20 in the control group. The average weight-loss difference was only about three pounds (1.3 kg), but those who claimed to have actually complied with the three-times-a-day instructions lost about eight more pounds (4.3 kg) compared to those who only drank the extra water once a day or less. This is comparable to commercial weight-loss programs, like Weight Watchers, and all the participants did was drink some extra water.
The video I mentioned is The New Calories per Pound of Weight Loss Rule.
If you missed my previous video, see The Effect of Drinking Water on Adrenal Hormones.
For all the specifics, check out Optimizing Water Intake to Lose Weight, coming up next.
October 31, 2024
Does Drinking Water Affect Our Adrenal Hormones?
Drinking water can be a safe, simple, and effective way to prevent yourself from fainting.
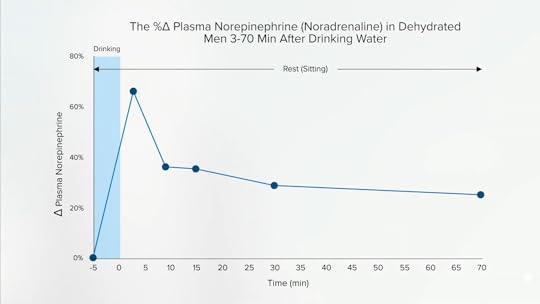
Within three minutes of drinking a few cups of water (12 mL/kg of body weight), the level of the adrenal gland hormone noradrenaline in our bloodstream can shoot up by 60 percent, as you can see in the graph below and at 0:19 in my video The Effect of Drinking Water on Adrenal Hormones.
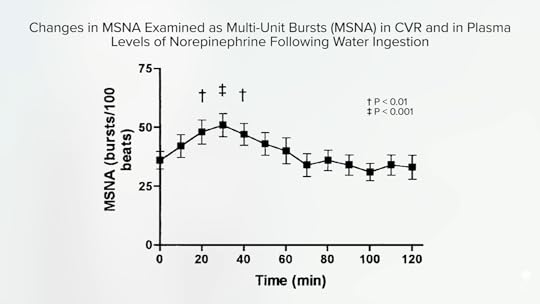
When researchers had people drink two cups (500 mL) of water with electrodes on their legs, about a 40 percent increase in bursts of fight-or-flight nerve activity within 20 minutes was documented, as shown in the graph below and at 0:25 in my video.

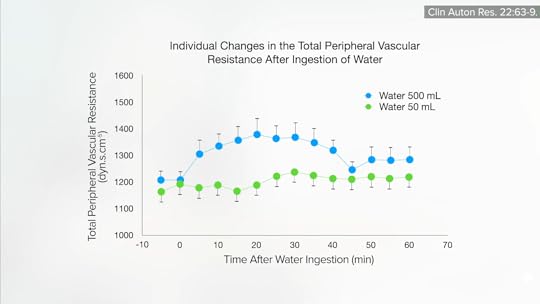
If you drink two or three cups (11 mL/kg of body weight) of water, blood flow squeezes down in your arms and calves, clamping down nearly in half, as the arteries to your limbs and skin constrict to divert blood to your core, as you can see in the graph below and at 0:42 in my video. That’s why drinking water can be such a safe, simple, and effective way to prevent yourself from fainting, which is known medically as syncope.

Fainting is “the sudden brief loss of consciousness caused by diminished cerebral blood flow,” that is, to the brain. About one in five people experience this at least once, and about one in ten may have repeated episodes. It’s the cause of millions of emergency room visits and hospitalizations every year. Though fainting can be caused by heart problems, it is most often triggered by prolonged standing (because blood pools in our legs) or strong emotions, which can cause our blood pressure to bottom out.
About 1 in 25 people has what’s called blood-injury-injection phobia, where getting a needle stick, for example, can cause you to faint. More than 150,000 people experience fainting or near-fainting spells each year when they donate blood. To help prevent yourself from getting woozy, try drinking two cups of water (500 mL) five minutes before getting stuck with the needle. The secret isn’t in bolstering your overall blood volume. If you drink two cups of water or even a whole quart (500 to 1,000 mL), your blood volume doesn’t change by more than 1 or 2 percent. Rather, it’s due to the shift in the distribution of blood toward your center, caused by the noradrenaline-induced peripheral artery constriction, as you can see in the graph below and at 1:56 in my video.
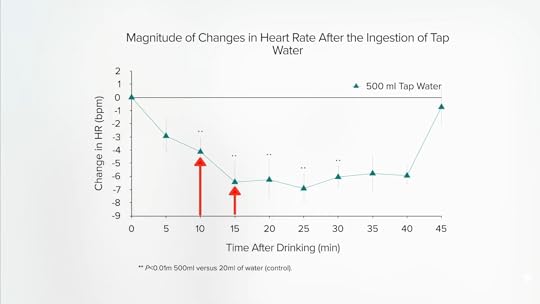
Drinking water stimulates as much noradrenaline release as drinking a couple cups of coffee or smoking a couple unfiltered cigarettes. If the simple act of drinking water causes such a profound fight-or-flight reaction, why doesn’t it cause our heart to pound and shoot our blood pressure through the roof? It’s like the diving reflex I talked about in my previous video. When we drink water, our body simultaneously sends signals to our heart to slow it down, to “still your beating heart.” You can try it at home: Measure your heart rate before and after drinking two cups (500 mL) of water. Within ten minutes, your heart rate should slow by about four beats per minute. By 15 minutes, you should be down by six or seven beats, as you can see in the graph below and at 2:42 in my video.
One of the ways scientists figured this out was by studying heart transplant patients. When you move a heart from one person to another, you have to sever all the attached nerves. Amazingly, some of the nerves grow back. But still, if you give healed heart transplant patients two glasses of water, their blood pressure goes up as much as 29 points. The body is unable to sufficiently quell the effect of that burst of noradrenaline. Some people have a condition known as autonomic failure, in which blood pressure regulation nerves don’t work properly and their pressures can skyrocket dangerously by more than 100 points after drinking about two cups (480 mL) of water. That’s how powerful an effect the simple act of drinking water can be. The only reason that doesn’t happen to all of us is that we have an even more powerful counter-response to keep our hearts in check. (This reminds me of the woman who had a stroke after taking the ice bucket challenge due to an insufficient diving reflex to tamp down all that extra noradrenaline release.)
This remarkable water effect can be useful for people suffering from milder forms of autonomic failure, such as orthostatic hypotension, which is when people get dizzy after standing up suddenly. Drinking some water before getting out of bed in the morning can be a big help. What about that metabolic boost, though? With so much noradrenaline being released and your adrenal gland hormones in overdrive, might drinking a few glasses of water cause you to burn more body fat? Could tap water be a safe form of ephedra, giving us all the weight loss but with a nice slowing of our heart rate instead? Researchers decided to put it to the test, which we’ll explore next.
If you missed the previous video, check out How to Get the Weight Loss Benefits of Ephedra Without the Risks.
Stay tuned for What Is the Safest Metabolism Booster? and Friday Favorites: Optimizing Water Intake to Lose Weight.
What kind of water is better? Find out in Is it Best to Drink Tap, Filtered, or Bottled Water?.
October 29, 2024
Ephedra-Like Weight Loss Minus the Risks
The diving reflex shows that it’s possible to have selective adrenal hormone effects.
Thermogenic drugs like DNP can cause people to overheat to death; they can increase resting metabolic rates by 300 percent or more. A more physiological spread would range about ten times less, from a 30 percent slower metabolism in people with an underactive thyroid to a 30 percent higher metabolism when the part of our nervous system that controls our fight-or-flight response is activated. In response to a fright or acute stress, special nerves release a chemical called noradrenaline to ready us for confrontation. We experience this by our skin getting paler, cold, and clammy, as blood is diverted to our more vital organs. Our mouth can get dry as our digestive system is put on hold, and our heart starts to beat faster. What we don’t feel is the extra fat being burned to liberate energy for the fight.
That’s why people started taking ephedra for weight loss—“to stimulate the release of noradrenaline from nerve endings.”
Ephedra is an evergreen shrub. It’s been used in China for thousands of years to treat asthma because it causes that same release of noradrenaline that offers relief to people with asthma by dilating their airways. In the United States, it was appropriated for use as a metabolic stimulant, shown to result in about 2 pounds (0.9 kg) of weight loss a month in 19 placebo-controlled trials. By the late 1990s, millions of Americans were taking it. The problem is that it also had all the other noradrenaline effects, like increasing heart rate and blood pressure. So, chronic use resulted in “stroke, cardiac arrhythmia, and death.” The U.S. Food and Drug Administration warned of its risks in 1994, but ephedra wasn’t banned until a decade later after a 23-year-old Major League Baseball pitcher dropped dead. His “autopsy report revealed evidence of ephedra, which the medical examiner said contributed to his death.”
In the current Wild West of dietary supplement regulation, not only can a supplement be “marketed without any safety data” at all, but the manufacturer is under no obligation to disclose adverse effects that may arise. No surprise, then, that online vendors assured absolute safety: “No negative side effects to date.” “No adverse side-effects, no nervous jitters or underlying anxiety, no moodiness…” “100% safe for long-term use.” “It will not interact with medications and has no harmful side effects.” The president of Metabolife International, a leading seller of ephedra, assured the FDA that the company had never received a single “notice from a consumer that any serious adverse health event has occurred…” In reality, it had received about 13,000 health complaints, including reports of serious injuries, hospitalizations, and even deaths.
If only there were a way to get the good without the bad. As I discuss in my video How to Get the Weight Loss Benefits of Ephedra Without the Risks, there is. But to understand it, you first have to grasp a remarkable biological phenomenon known as the diving reflex.
Imagine walking across a frozen lake and suddenly falling through the ice, plunging into the freezing depths. It’s hard to think of a greater, instantaneous fight-or-flight shock than that. Indeed, noradrenaline would be released, causing the blood vessels in your arms and legs to constrict to bring blood back to your core. You can imagine how fast your heart might start racing, but that would be counterproductive because you’d use up your oxygen faster. Remarkably, what happens instead is your heart rate slows down. That’s the diving reflex, first described in the 1700s. Air-breathing animals are born with this automatic safety feature to help keep us from drowning.
In medicine, we can exploit this physiological quirk with what’s called a “cold face test.” To determine if a comatose patient has intact neural pathways, you can apply cold compresses to their face to see if their heart immediately starts slowing down. Or, more dramatically, it can be used to treat people who flip into an abnormally rapid heartbeat. Remember that episode of ER where Carter dunked a patient’s face into a tray of ice water? (That show aired on TV when I was in medical school, and a group of us would gather around and count how many times they violated “universal precautions.”)
What does this have to do with weight loss? The problem with noradrenaline-releasing drugs like ephedra is the accompanying rise in heart rate and blood pressure. What the diving reflex shows is that it’s possible to experience selective noradrenaline effects, raising the possibility that there may be a way to get the metabolic boost without the risk of stroking out. Unbelievably, this intricate physiological feat may be accomplished by the simplest of acts: Instead of drowning in water, simply drink it. Really? Yes, you can boost your metabolism by drinking water. Buckle your safety belts because you are in for a wild ride—one that continues next.
This is the first in a four-part video series. Stay tuned for:
The Effect of Drinking Water on Adrenal Hormones What Is the Safest Metabolism Booster? Friday Favorites: Optimizing Water Intake to Lose WeightYou may also be interested in Friday Favorites: The Best Diet for Weight Loss and Disease Prevention.
October 24, 2024
Epigenetics and Obesity
Identical twins don’t just share DNA; they also share a uterus. Might that help account for some of their metabolic similarities? “Fetal overnutrition, evidenced by large infant birth weight for gestational age, is a strong predictor of obesity in childhood and later life.” Could it be that you are what your mom ate?
A dramatic illustration from the animal world is the crossbreeding of Shetland ponies with massive draft horses. Either way, the offspring are half pony/half horse, but when carried in the pony uterus, they come out much smaller, as you can see below and at 0:47 in my video The Role of Epigenetics in the Obesity Epidemic. (Thank heavens for the pony mother!) This is presumably the same reason why the mule (horse mom and donkey dad) is larger than the hinny (donkey mom and horse dad). The way you test this in people is to study the size of babies from surrogates after in vitro fertilization.

Who do you think most determines the birth weight of a test-tube baby? Is it the donor mom who provided all the DNA or the surrogate who provided the intrauterine environment? When it was put to the test, the womb won. Incredibly, a baby who had a thin biological mother but was born to a surrogate with obesity may harbor a greater risk of becoming obese than a baby with a heavier biological mother but born to a slim surrogate. The researchers “concluded that the environment provided by the human mother is more important than her genetic contribution to birth weight.”
The most compelling data come from comparing obesity rates in siblings born to the same mother, before and after her bariatric surgery. Compared to their brothers and sisters born before the surgery, those born when mom weighed about 100 pounds less had lower rates of inflammation, metabolic derangements, and, most critically, three times less risk of developing severe obesity—35 percent of those born before the weight loss were affected, compared to 11 percent born after. The researchers concluded that “these data emphasize how critical it is to prevent obesity and treat it effectively to prevent further transmission to future generations.”
Hold on. Mom had the same DNA before and after surgery. She passed down the same genes. How could her weight during pregnancy affect the weight destiny of her children any differently? Darwin himself admitted, “In my opinion, the greatest error which I have committed, has been not allowing sufficient weight to the direct action of the environment, i.e. food…independently of natural selection.” We finally figured out the mechanism by which this can happen—epigenetics.
Epigenetics, which means “above genetics,” layers an extra level of information on top of the DNA sequence that can be affected by our surroundings, as well as potentially passed on to our children. This is thought to explain the “developmental programming” that can occur in the womb, depending on the weight of the mother—or even the grandmother. Since all the eggs in your infant daughter’s ovaries are already preformed before birth, a mother’s weight status during pregnancy could potentially affect the obesity risk of her grandchildren, too. Either way, you can imagine how this could result in an intergenerational vicious cycle where obesity begets obesity.
Is there anything we can do about it? Well, breastfed infants may be at lower risk for later obesity, though the benefits may be confined to those who are exclusively breastfed, as the effect may be due to growth factors triggered by exposure to the excess protein in baby formula, as you can see below and at 3:51 in my video. The breastfeeding data are controversial, though, with charges leveled of a “white hat bias.” That’s the concern that public health researchers might disproportionally shelve research results that don’t fit some goal for the greater good. (In this case, preferably publishing breastfeeding studies showing more positive results.) But, of course, that criticism came from someone who works for an infant formula company. Breast is best, regardless. However, its role in the childhood obesity epidemic remains arguably uncertain.

Prevention may be the key. Given the epigenetic influence of maternal weight during pregnancy, a symposium of experts on pediatric nutrition concluded that “planning of pregnancy, including prior optimization of maternal weight and metabolic condition, offers a safe means to initiate the prevention rather than treatment of pediatric obesity.” Easier said than done, but overweight moms-to-be may take comfort in the fact that after the weight loss in the surgery study, even the moms who gave birth to kids with three times lower risk were still, on average, obese themselves, suggesting weight loss before pregnancy is not an all-or-nothing proposition.
What triggered the whole obesity epidemic to begin with? There are a multitude of factors, and I covered many of them in my 11-video series on the epidemic in the related posts below.
We are what our moms ate in other ways, too. Check out:
Heart Disease May Start in the Womb Maternal Diet May Affect Stress Responses in Children Flashback Friday: The Effect of Animal Protein on Stress Hormones, Testosterone, and PregnancyOctober 22, 2024
Treat Type 1 Diabetes with a Plant-Based Diet?
Is it possible to reverse type 1 diabetes if caught early enough?
The International Journal of Disease Reversal and Prevention has already had its share of miraculous disease reversals with a plant-based diet. For instance, one patient began following a whole food, plant-based diet after having two heart attacks in two months. Within months, he experienced no more chest pain, controlled his cholesterol, blood pressure, and blood sugars, and also lost 50 pounds as a nice bonus. Yet, the numbers “do not capture the patient’s transformation from feeling like a ‘dead man walking’ to being in command of his health with a new future and life.”
I’ve previously discussed cases of reversing the autoimmune inflammatory disease psoriasis and also talked about lupus nephritis (kidney inflammation). What about type 1 diabetes, an autoimmune disease we didn’t think we could do anything about? In contrast to type 2 diabetes, which is a lifestyle disease that can be prevented and reversed with a healthy enough diet and lifestyle, type 1 diabetes is an autoimmune disease in which our body attacks our pancreas, killing off our insulin-producing cells and condemning us to a life of insulin injections—unless, perhaps, it’s caught early enough. If a healthy enough diet is started early enough, might we be able to reverse the course of type 1 diabetes by blunting that autoimmune inflammation?
As I discuss in my video Type 1 Diabetes Treatment: A Plant-Based Diet, we know that patients with type 1 diabetes “may be able to reduce insulin requirements and achieve better glycemic [blood sugar] control” with healthier diets. For example, children and teens were randomized to a nutritional intervention in which they increased the whole plant food density of their diet—meaning they ate more whole grains, whole fruits, vegetables, legumes (beans, split peas, chickpeas, and lentils), nuts, and seeds. Researchers found that the more whole plant foods, the better the blood sugar control.
The fact that more whole fruits were associated “with better glycemic [blood sugar] control has important clinical implications for nutrition education” in those with type 1 diabetes. We should be “educating them on the benefits of fruit intake, and allaying erroneous concerns that fruit may adversely affect blood sugar.”
The case series in the IJDRP, however, went beyond proposing better control of just their high blood sugars, the symptom of diabetes, but better control of the disease itself, suggesting the anti-inflammatory effects of whole healthy plant foods “may slow or prevent further destruction of the beta cells”—the insulin-producing cells of the pancreas—“if dietary intervention is initiated early enough.” Where did this concept come from?
A young patient. Immediately following diagnosis of type 1 diabetes at age three, a patient began a vegetable-rich diet and, three years later, “has not yet required insulin therapy…and has experienced a steady decline in autoantibody levels,” which are markers of insulin cell destruction. Another child, who also started eating a healthier diet, but not until several months after diagnosis, maintains a low dose of insulin with good control. And, even if their insulin-producing cells have been utterly destroyed, individuals with type 1 diabetes can still enjoy “dramatically reduced insulin requirements,” reduced inflammation, and reduced cardiovascular risk, which is their number one cause of death over the age of 30. People with type 1 diabetes have 11 to 14 times the risk of death from cardiovascular disease compared to the general population, and it’s already the top killer among the public, so it’s closer to 11 to 14 times more important for those with type 1 diabetes to be on the only diet and lifestyle program ever proven to reverse heart disease in the majority of patients—one centered around whole plant foods. The fact it may also help control the disease itself is just sugar-free icing on the cake.
All this exciting new research was presented in the first issue of The International Journal of Disease Reversal and Prevention. As a bonus, there’s a companion publication called the Disease Reversal and Prevention Digest. These are for the lay public and are developed with the belief I wholeheartedly share that “everyone has a right to understand the science that could impact their health.” You can go behind the scenes and hear directly from the author of the lupus series, read interviews from luminaries like Dean Ornish, see practical tips from dietitians on making the transition towards a healthier diet, and enjoy recipes.
The second issue includes more practical tips, such as how to eat plant-based on a budget, and gives updates on what Dr. Klaper is doing to educate medical students, what Audrey Sanchez from Balanced is doing to help change school lunches, and how Dr. Ostfeld got healthy foods served in a hospital. (What a concept!) And what magazine would be complete without an article to improve your sex life?
The journal is free, downloadable at IJDRP.org, and its companion digest, available at diseasereversaldigest.com, carries a subscription fee. I am a proud subscriber.
Want to learn more about preventing type 1 diabetes in the first place? See the related posts below.
October 17, 2024
Eating an Anti-Inflammatory Diet for Lupus
Green smoothies are put to the test for the autoimmune disease lupus.
There are dozens and dozens of journals I try to stay on top of every month, and one I always anticipate is The International Journal of Disease Reversal and Prevention, a peer-reviewed medical “journal created to document the science of nutrition and lifestyle to prevent, suspend and reverse disease,” with an editor-in-chief no less prestigious than Dr. Kim Williams, past president of the American College of Cardiology. I was honored to join its editorial advisory board, along with so many of my heroes. The best part? It’s free. Go to IJDRP.org and put in your email to subscribe at no cost, and you’ll be alerted when new issues are out, which you can download in full in PDF form. (Did I mention it’s free?)
When it comes to chronic lifestyle diseases, wrote Dr. Williams, “Instead of preventing chronic lifestyle diseases, we [doctors] manage. Never cure, just mitigate. Why? Because of finance, culture, habit, and tradition.” There are many of us, though, who “envision a world where trillions of dollars are not spent on medical care that should never have been necessary, but rather on infrastructure, environment, education, and advancing science. For this reason, comes The International Journal of Disease Reversal and Prevention (IJDRP).” After all, wrote the journal’s co-founder, “Without data, you’re just another person with an opinion.”
To give you a taste of the journal: How about pitting plants against one of the most inflammatory diseases out there—lupus, an autoimmune disease in which your body can start attacking your DNA? Kidney inflammation is a common consequence, and even with our armamentarium of immunosuppressant drugs and steroids, lupus-induced kidney inflammation can lead to end-stage renal disease, which means dialysis, and even death. That is, unless you pack your diet with some of the most anti-inflammatory foods out there and your kidney function improves so much you no longer need dialysis or a kidney transplant. Another similar case was presented with a resolution in symptoms and normal kidney function, unless the patient deviated from the diet and his symptoms then reappeared.
As I discuss in my video Anti-Inflammatory Diet for Lupus, even just cutting out animal products can make a difference. Researchers randomized people to remove meat, eggs, and dairy from their diets without significantly increasing fruit and vegetable intake and found that doing just that can lower C-reactive protein levels by nearly a third within eight weeks, as you can see below and at 2:21 in my video. (Our C-reactive protein level is a sensitive indicator of whole-body inflammation.)

But with lupus, the researchers didn’t mess around. Each day, the study subjects were to eat a pound of leafy greens and cruciferous vegetables like kale, fruits like berries, and lots of chia or flax, and drink a gallon of water. We’re talking about a green smoothie diet to extinguish lupus flares. (Note, though, that if your kidneys are already compromised, this should be done under physician supervision so they can monitor your electrolytes like potassium and make sure you don’t get overloaded with fluid.) Bottom line? With such remarkable improvements due to dietary changes alone, the hope is that researchers will take up the mantle and formally put it to the test.
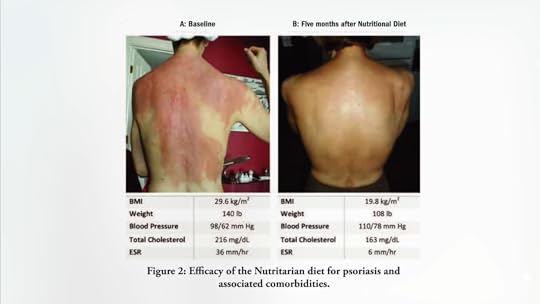
Reversals of autoimmune inflammatory skin disease can be particularly striking visually. A woman with a 35-year history of psoriasis that had been unsuccessfully managed for 19 years with drugs suffered from other autoimmune conditions, including Sjogren’s syndrome. She was put on an extraordinarily healthy diet packed with greens and other vegetables, fruits, nuts, seeds, avocados, and some whole grains, and boom! Within one year, she went from 40 percent of her entire body surface area inflamed and affected down to 0 percent, completely clear, and, as a bonus, her Sjogren’s symptoms resolved, too, while helping to normalize her weight and cholesterol. You can see before and after photos below and at 3:39 in my video.
I think I only have one other video on lupus: Fighting Lupus with Turmeric: Good as Gold. It’s not for lack of trying, though. There just hasn’t been much research out there.
I talk about another autoimmune disease, type 1 diabetes, in Type 1 Diabetes Treatment: A Plant-Based Diet.
To read and subscribe—for free—to The International Journal of Disease Reversal and Prevention, visit www.IJDRP.org.
October 15, 2024
Spend Time in Nature for Your Health?
For perhaps 99.99 percent of our time as a species on Earth, we lived outdoors in the natural environment. Might there be a health benefit to returning now and again, and surrounding ourselves with nature? That’s a question that urban planners have asked. “Are people living in greener areas healthier than people living in less green areas?” Should we put it in a park or another car park?
“In a greener environment, people report fewer symptoms of illness and have better perceived general health. Also, people’s mental health appears to be better”—and by a considerable amount. Indeed, “assuming a causal relation between greenspace and health, 10% more greenspace in the living environment leads to a decrease in the number of symptoms that is comparable with a decrease in age by 5 years.” That is a big assumption, though.
Still, you could imagine some potential mechanisms of why it could be. It could mean less air pollution, and air pollution is no joke. It is the fifth leading cause of death on our planet, killing about five million people a year. Though, of course, our number one risk factor is our diet, which kills twice as many individuals, as you can see below and at 1:18 in my video Are There Health Benefits of Spending Time in Nature?.

So, it could be an antipollution effect, or maybe there’s something special about experiencing greenspaces beyond them just offering more opportunities to exercise. The simplest explanation is probably that a natural setting “simply promotes health-enhancing behavior rather than having specific and direct benefits for health.” It’s harder to go jogging in the park when there is no park. Ironically, it seems that even when people have access to nature, they don’t necessarily take advantage of it. And, even if there were a link, “a question remains about the possibility of a ‘self-selection’ phenomenon: do natural environments elicit increased physical activity and well-being, or do physically active individuals choose to live in areas with more opportunities for physical activity?” What I wanted to know is, “apart from the promotion of physical activity,” are there “added benefits to health of exposure to natural environments”?
Now certainly, just being exposed to sunlight can treat things like seasonal affective disorder and provide vitamin D, the sunshine vitamin, but are there any other inherent benefits? You don’t know until you put it to the test. Some of the studies are just silly, though. Consider “Relationships Between Vegetation in Student Environments and Academic Achievement Across the Continental U.S.” At first, I thought the study was about academic achievement and vegetarianism, but no—it’s about vegetation. Researchers found a “positive relationship between non-forest vegetation and graduation rates for schools.” Maybe the Ivy League’s edge is from the ivy?
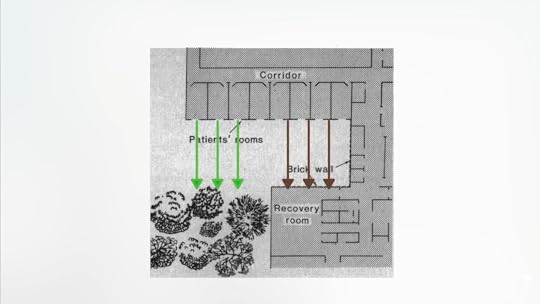
The study entitled “View Through a Window May Influence Recovery from Surgery” starts to make things more interesting. As you can see below and at 3:04 in my video, some patient rooms at a suburban hospital looked out at trees, while others to a brick wall. “Twenty-three surgical patients assigned to rooms with windows looking out on a natural scene had shorter postoperative hospital stays…and took fewer potent analgesics [painkillers] than 23 matched patients in similar rooms with windows facing a brick building wall.” You can’t chalk that up to a vitamin D effect.
What could it be about just looking at trees? Maybe it is the “vitamin G”—just the color of green. We know how healthy it is to eat our greens. What about just looking at them? Researchers had people exercise while watching a video simulating going through a natural, green-colored setting, the same video in black and white, or everything tinted red, and no differences were noted (with the exception that red made people feel angry), as you can see below and at 3:46 in my video.

The most interesting mechanism that has been suggested that I’ve run across is fractals. Have you ever noticed that “for example, in a tree, all the branches—from big to small—are scaled-down versions of the entire tree”? Each branch has a shape similar to the whole tree itself. Fractal patterns are found throughout nature, where you see “a cascade of self-similar patterns over a range of magnification scales, building visual stimuli that are inherently complex.” And, as you can see when you’re hooked up to an EEG, our brain seems to like them, too.
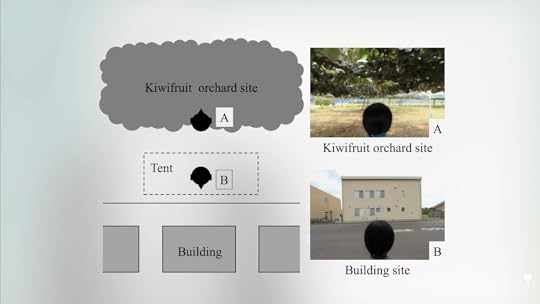
Regardless of the mechanism, if you compile all the controlled studies on using nature as a health promotion intervention, you tend to see mostly psychological benefits, whereas the findings related to physical outcomes were less consistent. “The most common type of study outcome was self-reported measures of different emotions.” For instance, what makes you feel better: staring at a kiwifruit orchard or a building? (See below and 4:41 in my video.) Awkwardly described, thanks presumably to the language barrier, as a comparison of “synthetic versus organic stimulation.”
As you can see below and at 5:00 in my video, natural settings may make people more attentive and less sad, but when it comes to some objective measures like blood pressure, no significant effect was found. People who exercise outdoors often say they feel great, “suggesting that green exercise activities can increase…various psychological subscales,” such as “mood, focus, and energy”—within just five or so minutes of being out in the woods.

Yet these studies tended not to be randomized trials. Researchers just asked people who already sought out nature what they thought about nature, so it’s no wonder they like it—otherwise, they wouldn’t be out there. But nature-based interventions are low-cost, often free, in fact, and non-invasive (unless you count the mosquitoes). So, if you want “a natural high,” I say go for it, whatever makes you happy. (Not all green exercisers like trees. Golfers just viewed them as obstacles.)
For more on air pollution, see my videos Best Food to Counter the Effects of Air Pollution and The Role of Pesticides and Pollution in Autism.
Of course, there are benefits to any kind of exercise indoors or out. Check out the related posts below.